Brain Tumor Res Treat.
2014 Oct;2(2):128-131. 10.14791/btrt.2014.2.2.128.
Large Solid Hemangioblastoma in the Cerebellopontine Angle: Complete Resection Using the Transcondylar Fossa Approach
- Affiliations
-
- 1Department of Neurosurgery, Incheon St. Mary's Hospital, The Catholic University of Korea College of Medicine, Incheon, Korea. hymnsolmh@gmail.com
- KMID: 2134285
- DOI: http://doi.org/10.14791/btrt.2014.2.2.128
Abstract
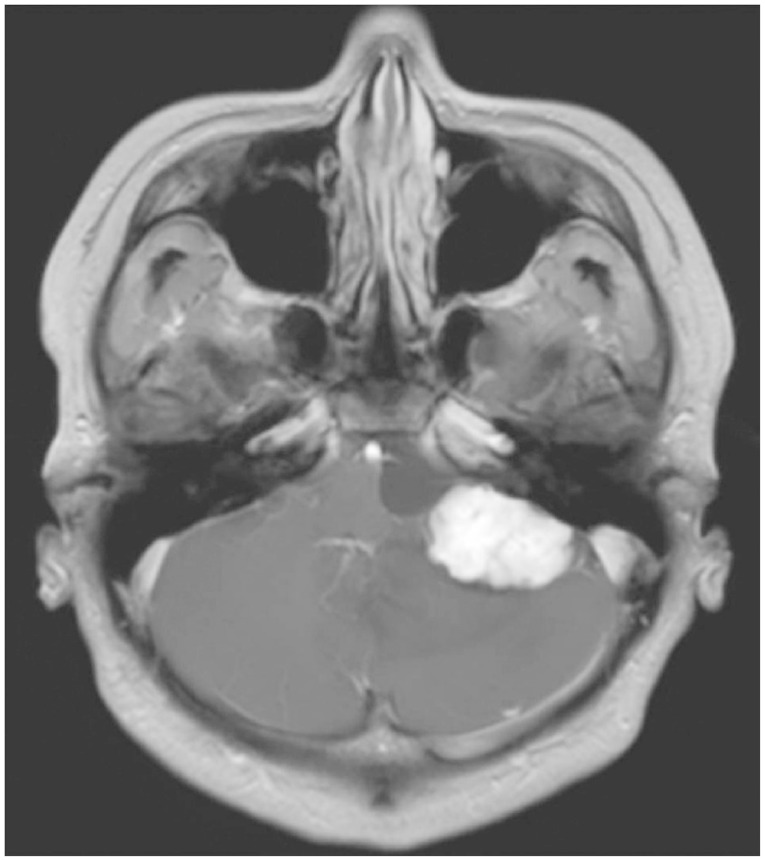
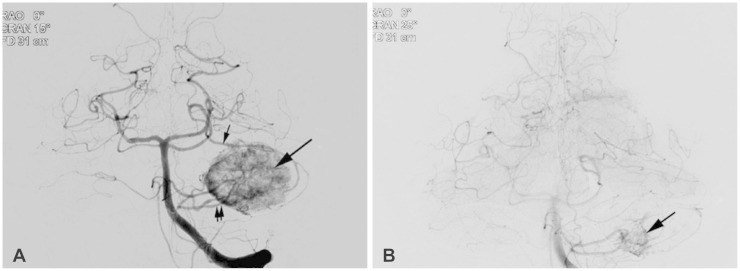
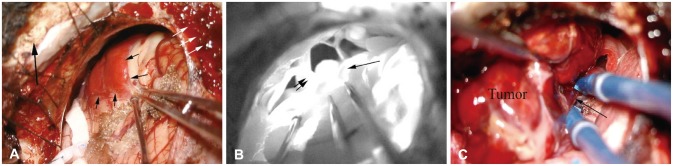
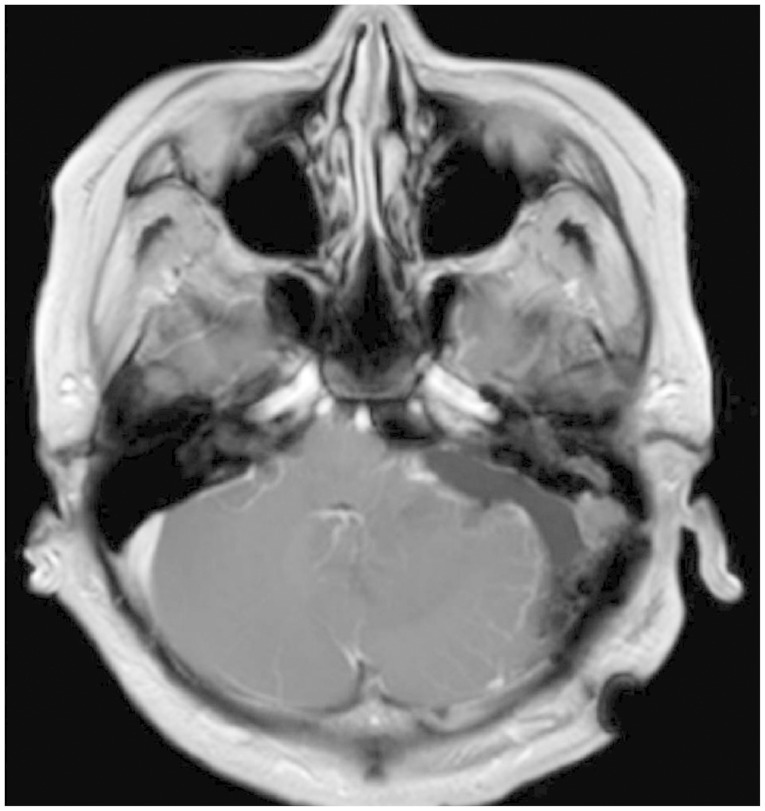
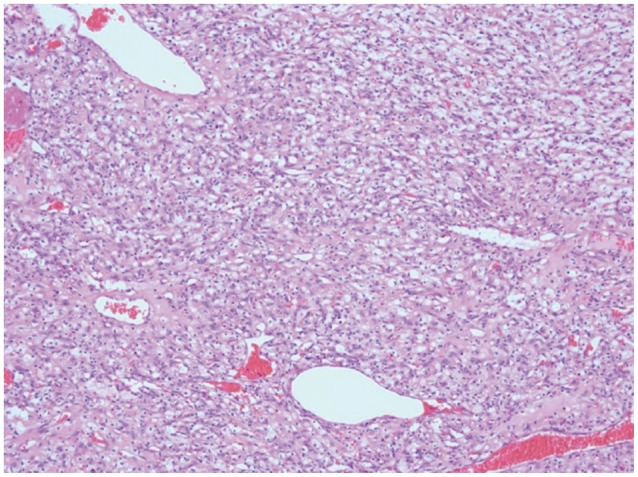
- Hemangioblastomas (HBMs) in the cerebellopontine angle (CPA) have rarely been reported. When they are within the CPA, they may be misdiagnosed as vestibular schwannoma (VS) or cystic meningioma. Therefore, differential diagnosis is important for the safe treatment of the lesion. Large solid HBMs, similar to intracranial arteriovenous malformations (AVMs), are difficult to surgically remove from an eloquent area because of their location and hypervascularity. We report a case of an HBM in the CPA, which manifested as a hearing impairment or VS. Similar to AVM surgery, the tumor was widely opened and removed en bloc without a new neurological complication using the modified transcondylar fossa approach without resection of the jugular tubercle. Accurate diagnosis, pre-operative embolization, and a tailored approach were essential for the safe treatment of the HBM in the CPA.
Keyword
MeSH Terms
Figure
Reference
-
1. Amano T, Tokunaga S, Shono T, et al. Cerebellar hemangioblastoma manifesting as hearing disturbance. Neurol Med Chir (Tokyo). 2009; 49:418–420. PMID: 19779288.2. Bush ML, Pritchett C, Packer M, Ray-Chaudhury A, Jacob A. Hemangioblastoma of the cerebellopontine angle. Arch Otolaryngol Head Neck Surg. 2010; 136:734–738. PMID: 20644074.
Article3. Deb P, Sahni H, Bhatoe HS. Cystic angiomatous meningioma in the cerebellopontine angle mimicking hemangioblastoma. J Cancer Res Ther. 2010; 6:560–563. PMID: 21358102.
Article4. Dow GR, Sim DW, O'Sullivan MG. Excision of large solid haemangioblastomas of the cerebellopontine angle by a skull base approach. Br J Neurosurg. 2002; 16:168–171. PMID: 12046738.
Article5. Kamitani H, Hirano N, Takigawa H, et al. Attenuation of vascularity by preoperative radiosurgery facilitates total removal of a hypervascular hemangioblastoma at the cerebello-pontine angle: case report. Surg Neurol. 2004; 62:238–243. discussion 243-4. PMID: 15336869.
Article6. Matsushima T, Kawashima M, Masuoka J, Mineta T, Inoue T. Transcondylar fossa (supracondylar transjugular tubercle) approach: anatomic basis for the approach, surgical procedures, and surgical experience. Skull Base. 2010; 20:83–91. PMID: 20808532.
Article7. Nair BR, Joseph V, Chacko G, Keshava SN. Giant solid hemangioblastoma of the cerebellopontine angle: a technically challenging case. Neurol India. 2014; 62:228–229. PMID: 24823754.
Article8. Qiao PF, Niu GM, Han XD. Hemangioblastoma originating from the right cerebellopontine angle. Neurosciences (Riyadh). 2011; 16:372–374. PMID: 21983384.9. Rachinger J, Buslei R, Prell J, Strauss C. Solid haemangioblastomas of the CNS: a review of 17 consecutive cases. Neurosurg Rev. 2009; 32:37–47. discussion 47-8. PMID: 18810515.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Four Cases of Large Cerebellopontine Angle Tumors Removed by Translabyrinthine Approach
- Retroamstoid Suboccipital Approch to Cerebellopontine Angle Tumors
- Surgical Anatomy for the Extended Middle Fossa Approach
- Traumatic Acute Subdural Hematoma Extending from the Posterior Cranial Fossa to the Cerebellopontine Angle
- Conbined approach for large tumor of cerebellopontine angle