J Korean Assoc Oral Maxillofac Surg.
2015 Dec;41(6):346-351. 10.5125/jkaoms.2015.41.6.346.
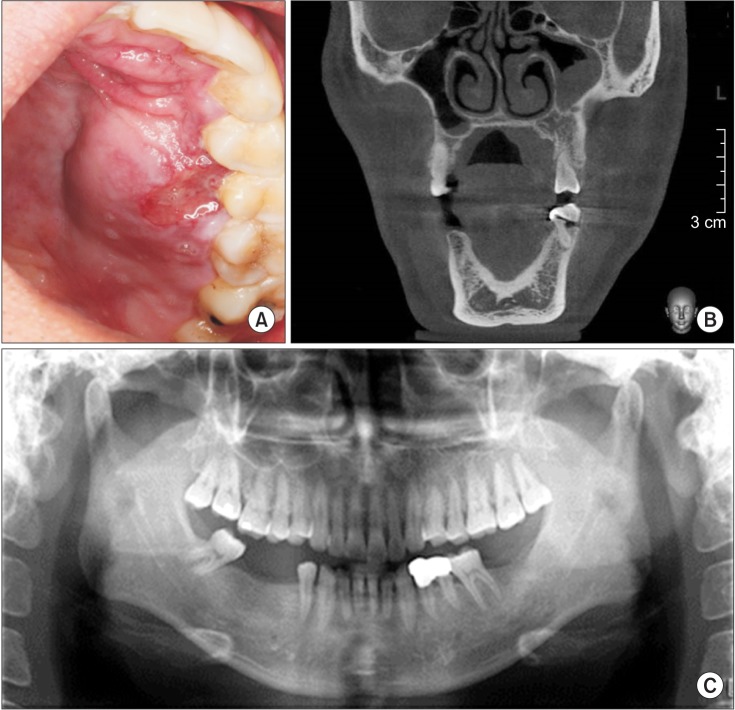
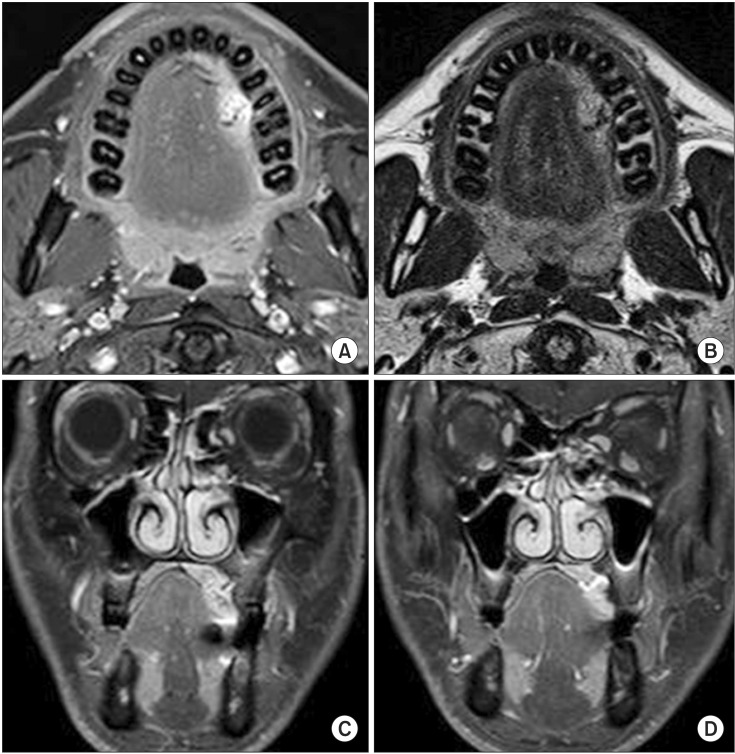
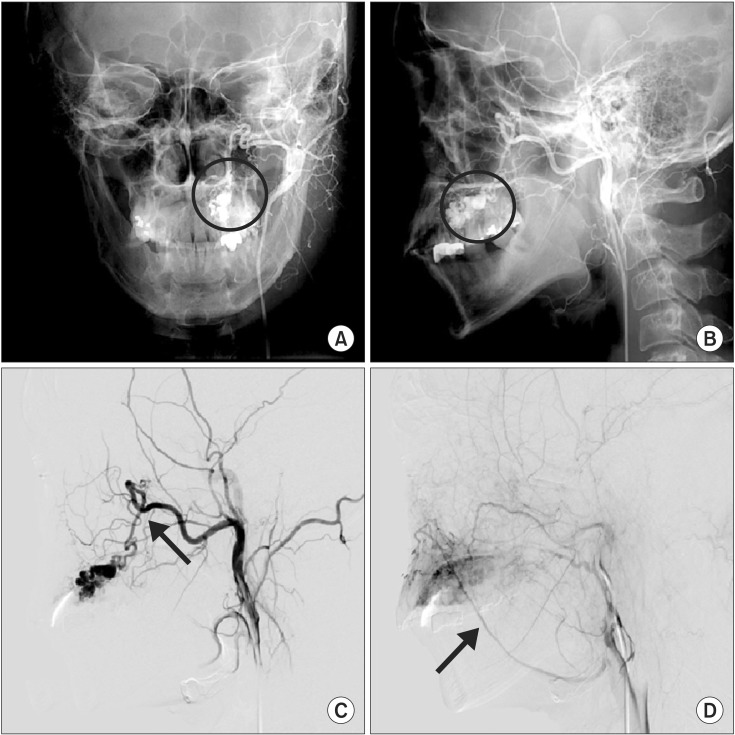
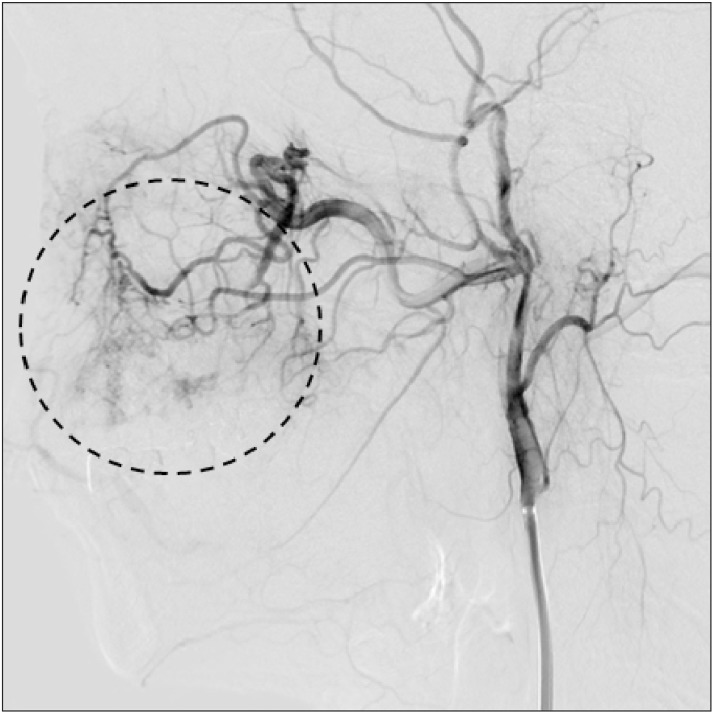
Recurrent arteriovenous malformation on palate after embolization combined surgical resection: preoperative magnetic resonance features and intraoperative angiographic findings
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, School of Dentistry, Pusan National University, Yangsan, Korea. ydkimdds@pusan.ac.kr
- 2Department of Radiology, Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Hospital, Pusan National University School of Medicine, Yangsan, Korea.
- KMID: 2133184
- DOI: http://doi.org/10.5125/jkaoms.2015.41.6.346
Abstract
- Angiography is the gold standard for the diagnosis and complete resection of arteriovenous malformations (AVMs). The absence of residual AVM after surgery is commonly believed to reduce the risk of future hemorrhage. However, AVMs can recur after proven complete angiographic resection can occur, albeit rarely, especially in the pediatric population. We report a rare case of a recurrent AVM two years after complete resection in an adult patient. This case report shows that AVMs in adults can recur despite their rarity and despite postoperative angiography confirming complete removal. Moreover, in this case, the recurrent AVM involved a new feeding vessel that was not involved with the initial lesion.
Keyword
Figure
Cited by 1 articles
-
Nasal septum angiofibroma: a rare condition with an unusual onset
Maria Carla Spinosi, Francesca D'Amico, Chiara Mezzedimi, Cristiana Bellan, Manuela Cirami, Ilaria Innocenti Paganelli
J Korean Assoc Oral Maxillofac Surg. 2019;45(1):43-47. doi: 10.5125/jkaoms.2019.45.1.43.
Reference
-
1. Chiu YW, Wu HT, Chen YW, Lui MT, Kao SY, Lo WL. A giant venous malformation of face and neck: a case report. Taiwan J Oral Maxillofac Surg. 2011; 22:110–117.2. Duncan IC, Fourie PA. Vascular malformations part 2: current classification of vascular malformations. South Afr J Radiol. 2004; 8:23–30.3. Shetty DC, Urs AB, Rai HC, Ahuja N, Manchanda A. Case series on vascular malformation and their review with regard to terminology and categorization. Contemp Clin Dent. 2010; 1:259–262. PMID: 22114434.4. Noreau G, Landry PP, Morais D. Arteriovenous malformation of the mandible: review of literature and case history. J Can Dent Assoc. 2001; 67:646–651. PMID: 11841745.5. Sonstein WJ, Kader A, Michelsen WJ, Llena JF, Hirano A, Casper D. Expression of vascular endothelial growth factor in pediatric and adult cerebral arteriovenous malformations: an immunocytochemical study. J Neurosurg. 1996; 85:838–845. PMID: 8893722.
Article6. Virchow R. Die krankhaften Geschwülste 1. Berlin: Hirschwald;1863.7. Choi DJ, Alomari AI, Chaudry G, Orbach DB. Neurointerventional management of low-flow vascular malformations of the head and neck. Neuroimaging Clin N Am. 2009; 19:199–218. PMID: 19442906.
Article8. Garzon MC, Huang JT, Enjolras O, Frieden IJ. Vascular malformations: part I. J Am Acad Dermatol. 2007; 56:353–370. PMID: 17317485.9. Richter GT, Friedman AB. Hemangiomas and vascular malformations: current theory and management. Int J Pediatr. 2012; 2012:645678. DOI: 10.1155/2012/645678. PMID: 22611412.
Article10. Anderson JH, Grisius RJ, McKean TW. Arteriovenous malformation of the mandible. Oral Surg Oral Med Oral Pathol. 1981; 52:118–125. PMID: 6943478.
Article11. Codd PJ, Mitha AP, Ogilvy CS. A recurrent cerebral arteriovenous malformation in an adult. J Neurosurg. 2008; 109:486–491. PMID: 18759581.
Article12. Jacobowitz GR, Rosen RJ, Rockman CB, Nalbandian M, Hofstee DJ, Fioole B, et al. Transcatheter embolization of complex pelvic vascular malformations: results and long-term follow-up. J Vasc Surg. 2001; 33:51–55. PMID: 11137923.
Article13. Weil AG, Li S, Zhao JZ. Recurrence of a cerebral arteriovenous malformation following complete surgical resection: a case report and review of the literature. Surg Neurol Int. 2011; 2:175. PMID: 22276230.
Article14. Klimo P Jr, Rao G, Brockmeyer D. Pediatric arteriovenous malformations: a 15-year experience with an emphasis on residual and recurrent lesions. Childs Nerv Syst. 2007; 23:31–37. PMID: 17053936.
Article15. Lee BB, Baumgartner I, Berlien HP, Bianchini G, Burrows P, Do YS, et al. International Union of Angiology. Consensus Document of the International Union of Angiology (IUA)-2013. Current concept on the management of arterio-venous management. Int Angiol. 2013; 32:9–36. PMID: 23435389.16. Spetzler RF, Hargraves RW, McCormick PW, Zabramski JM, Flom RA, Zimmerman RS. Relationship of perfusion pressure and size to risk of hemorrhage from arteriovenous malformations. J Neurosurg. 1992; 76:918–923. PMID: 1588424.
Article17. Gabriel EM, Sampson JH, Wilkins RH. Recurrence of a cerebral arteriovenous malformation after surgical excision: case report. J Neurosurg. 1996; 84:879–882. PMID: 8622165.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Successful Transarterial Embolization in Arteriovenous Malformation of Uterus
- Reconstruction of the Face Using Thoracodorsal Artery Perforator Free Flap after Resection of Arteriovenous Malformation
- Clinical Study According to the Modality of Treatment of Cerebral Arteriovenous Malformations
- Surgical management and reconstruction of facial arteriovenous malformations
- Experience with Arteriovenous Malformation: A Report of One Case