J Korean Assoc Oral Maxillofac Surg.
2015 Dec;41(6):293-298. 10.5125/jkaoms.2015.41.6.293.
Cervicofacial infection in a Nigerian tertiary health institution: a retrospective analysis of 77 cases
- Affiliations
-
- 1Department of Maxillofacial Surgery, Ahmadu Bello University Teaching Hospital, Zaria. benfometey@hotmail.com
- 2Department of Dental and Maxillofacial Surgery, University of Calabar Teaching Hospital, Calabar, Nigeria.
- KMID: 2133175
- DOI: http://doi.org/10.5125/jkaoms.2015.41.6.293
Abstract
OBJECTIVES
Infection involving the orbit, zygomatic space, lateral pharyngeal space, or hemifacial and oral floor phlegmon is referred to as cervicofacialvinfection (CFI). When diagnosis and/or adequate treatment are delayed, these infections can be life-threatening. Most cases are the result of odontogenic infections. We highlight our experiences in the management of this life-threatening condition.
MATERIALS AND METHODS
This was a retrospective study of patients who presented with CFI from December 2005 to June 2012 at the Oral and Maxillofacial Surgery Clinic or the Accident and Emergency Unit of Ahmadu Bello University Teaching Hospital (Zaria, Nigeria). The medical records of all patients who presented with either localized or diffuse infection of the maxillofacial soft tissue spaces were retrospectively collected. Data collected was analyzed using SPSS version 13.0 and are expressed as descriptive and inferential statistics.
RESULTS
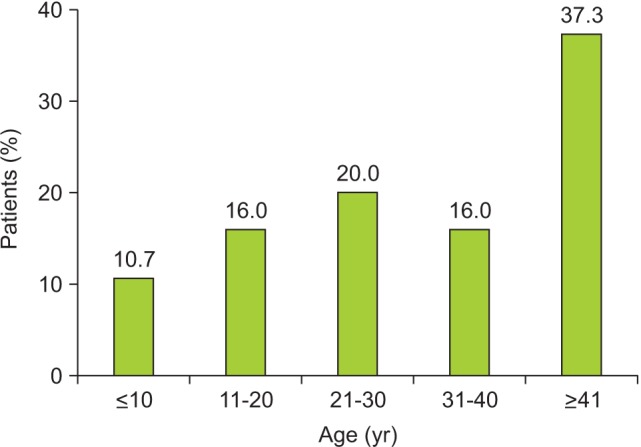
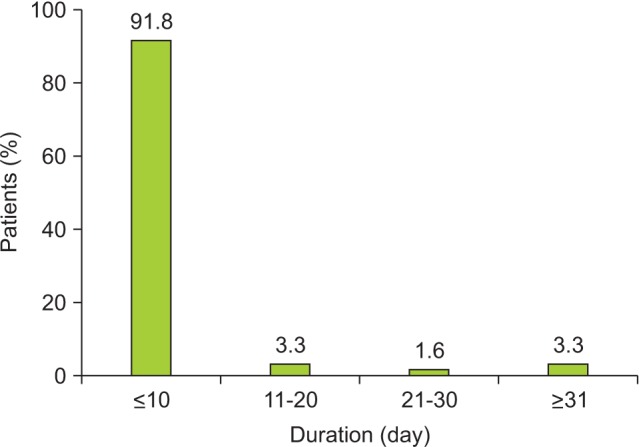
Of the 77 patients, 49 patients (63.6%) were males, a male to female ratio of 1:7.5. The ages ranged from two years to 75 years with a mean of 35.0+/-19.3 years, although most patients were older than 40 years. The duration of symptoms prior to presentation ranged from 6 to 60 days, with a mean of 11.0+/-9.4 days. More than 90% of the patients presented to the clinic within the first 10 days. The most commonly involved anatomical space was the submandibular space (n=29, 37.7%), followed by hemifacial space (n=22, 28.6%) and buccal space (n=7, 9.1%). Ludwig angina accounted for about 7.8% of the cases.
CONCLUSION
CFI most commonly involves the submandibular space, typically affects individuals with a low level of education, and is influenced by traditional medical practices. Despite improved health care delivery, CFI remains a significant problem in developing countries.
Keyword
MeSH Terms
Figure
Reference
-
1. Adekeye EO, Adekeye JO. The pathogenesis and microbiology of idiopathic cervicofacial abscesses. J Oral Maxillofac Surg. 1982; 40:100–106. PMID: 6950044.
Article2. Wang J, Ahani A, Pogrel MA. A five-year retrospective study of odontogenic maxillofacial infections in a large urban public hospital. Int J Oral Maxillofac Surg. 2005; 34:646–649. PMID: 15955663.
Article3. Bouloux GF, Wallace J, Xue W. Irrigating drains for severe odontogenic infections do not improve outcome. J Oral Maxillofac Surg. 2013; 71:42–46. PMID: 22726703.
Article4. Flynn Thomas R. Principles of management of odontogenic infections. In : Miloro M, Ghali GE, Larsen P, Waite P, editors. Peterson's principle of oral and maxillofacial surgery. 2nd ed. London, Hamilton: BC Decker Inc.;2004. p. 277–293.5. Mathew GC, Ranganathan LK, Gandhi S, Jacob ME, Singh I, Solanki M, et al. Odontogenic maxillofacial space infections at a tertiary care center in North India: a five-year retrospective study. Int J Infect Dis. 2012; 16:e296–e302. PMID: 22365137.
Article6. Boffano P, Roccia F, Pittoni D, Di Dio D, Forni P, Gallesio C. Management of 112 hospitalized patients with spreading odontogenic infections: correlation with DMFT and oral health impact profile 14 indexes. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 113:207–213. PMID: 22677738.
Article7. Cunningham LL Jr, Madsen MJ, Van Sickels JE. Using prealbumin as an inflammatory marker for patients with deep space infections of odontogenic origin. J Oral Maxillofac Surg. 2006; 64:375–378. PMID: 16487796.8. Poeschl PW, Spusta L, Russmueller G, Seemann R, Hirschl A, Poeschl E, et al. Antibiotic susceptibility and resistance of the odontogenic microbiological spectrum and its clinical impact on severe deep space head and neck infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 110:151–156. PMID: 20346713.
Article9. Farmahan S, Tuopar D, Ameerally PJ. The clinical relevance of microbiology specimens in head and neck space infections of odontogenic origin. Br J Oral Maxillofac Surg. 2014; 52:629–631. PMID: 24906248.
Article10. Storoe W, Haug RH, Lillich TT. The changing face of odontogenic infections. J Oral Maxillofac Surg. 2001; 59:739–748. PMID: 11429732.
Article11. Jundt JS, Gutta R. Characteristics and cost impact of severe odontogenic infections. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 114:558–566. PMID: 22819453.
Article12. Osunde OD, Akhiwu BI, Efunkoya AA, Adebola AR, Iyogun CA, Arotiba JT. Management of fascial space infections in a Nigerian teaching hospital: a 4-year review. Niger Med J. 2012; 53:12–15. PMID: 23271838.
Article13. Flynn TR, Shanti RM, Hayes C. Severe odontogenic infections, part 2: prospective outcomes study. J Oral Maxillofac Surg. 2006; 64:1104–1113. PMID: 16781344.
Article14. Ariji Y, Gotoh M, Kimura Y, Naitoh M, Kurita K, Natsume N, et al. Odontogenic infection pathway to the submandibular space: imaging assessment. Int J Oral Maxillofac Surg. 2002; 31:165–169. PMID: 12102414.
Article15. Gill Y, Scully C. Orofacial odontogenic infections: review of microbiology and current treatment. Oral Surg Oral Med Oral Pathol. 1990; 70:155–158. PMID: 2290641.
Article16. Adekeye EO, Brown AE, Adekeye JO. Cervicofacial abcesses of unknown origin: a survey of eighty-one cases. Oral Surg Oral Med Oral Pathol. 1978; 45:831–840. PMID: 355964.17. Fomete B, Ononiwu CN, Agbara R, Idehen OK, Okeke UA. Cervicofacial necrotizing fasciitis: case series and review of literature. Case Study Case Rep. 2013; 3:26–33.18. Gilmore WC, Jacobus NV, Gorbach SL, Doku HC, Tally FP. A prospective double-blind evaluation of penicillin versus clindamycin in the treatment of odontogenic infections. J Oral Maxillofac Surg. 1988; 46:1065–1070. PMID: 3142979.
Article19. Warnke PH, Becker ST, Springer IN, Haerle F, Ullmann U, Russo PA, et al. Penicillin compared with other advanced broad spectrum antibiotics regarding antibacterial activity against oral pathogens isolated from odontogenic abscesses. J Craniomaxillofac Surg. 2008; 36:462–467. PMID: 18760616.
Article20. Al-Qamachi LH, Aga H, McMahon J, Leanord A, Hammersley N. Microbiology of odontogenic infections in deep neck spaces: a retrospective study. Br J Oral Maxillofac Surg. 2010; 48:37–39. PMID: 19178989.
Article21. Fomete B, Saheeb BD, Obiadazie AC. A prospective clinical evaluation of the effects of chlorhexidine, warm saline mouth washes and microbial growth on intraoral sutures. J Maxillofac Oral Surg. 2015; 14:448–453. PMID: 26028872.
Article