Korean J Hepatobiliary Pancreat Surg.
2015 Nov;19(4):173-180. 10.14701/kjhbps.2015.19.4.173.
Comparative analysis of intraoperative radiofrequency ablation versus non-anatomical hepatic resection for small hepatocellular carcinoma: short-term result
- Affiliations
-
- 1Department of surgery, Chungnam National University Hospital, Daejeon, Korea. oxali@hanmail.net
- KMID: 2130970
- DOI: http://doi.org/10.14701/kjhbps.2015.19.4.173
Abstract
- BACKGROUNDS/AIMS
To compare the clinical outcomes of intraoperative radiofrequency ablation (RFA) and non-anatomical hepatic resection (NAHR) for small hepatocellular carcinoma (HCC).
METHODS
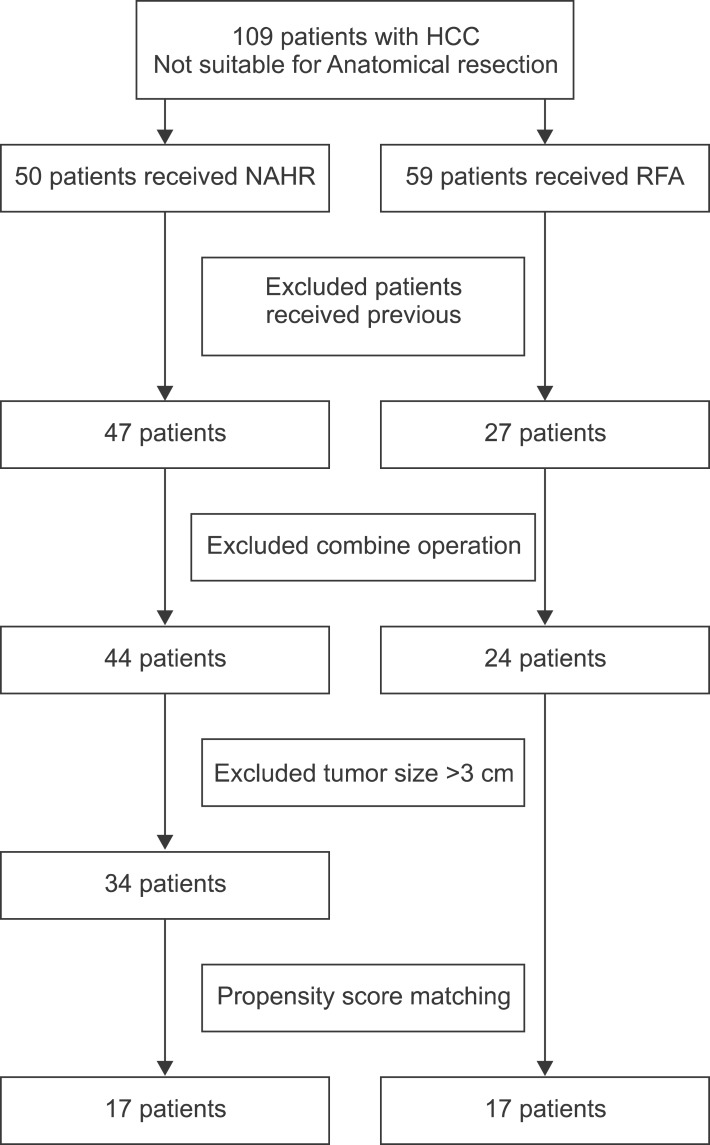
From February 2007 to January 2015, clinical outcomes of thirty four patients with HCC receiving RFA or NAHR were compared, retrospectively.
RESULTS
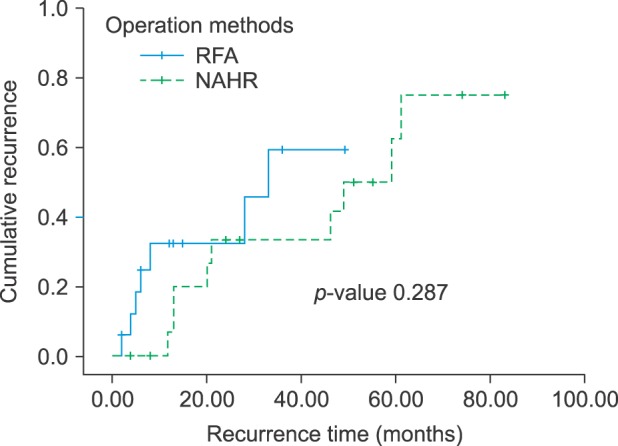
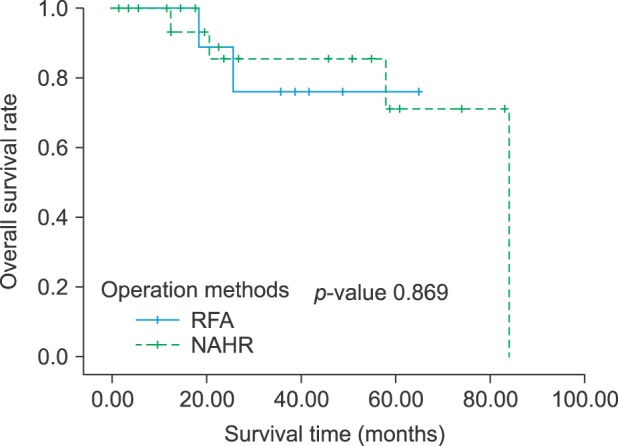
There was no difference of patient and tumor characteristic between the two groups that received RFA or NAHR. The 1, 2, and 3-year recurrence rates following RFA were 32.2%, 32.2% and 59.3% respectively, and 6.7%, 33.3% and 33.3% following NAHR respectively (p=0.287). The 1, 2 and 3-year overall survival (OS) rates following RFA were 100%, 88.9% and 76.2% respectively, and 100%, 85.6% and 85.6%, respectively, following NAHR (p=0.869). We did not find a definite statistical difference in recurrence rate and OS rate between the two groups. In the multivariate analysis, number of tumor was an independent prognostic factor for recurrence and albumin was an independent prognostic factor for OS.
CONCLUSIONS
We recommend non-anatomical hepatic resection rather than intraoperative RFA in small sized HCC, due to a higher recurrence rate in intraoperative RFA. Intraoperative RFA was inferior to non-anatomical hepatic resection in terms of recurrence rate. We need to select the optimal treatment considering liver function and possibility of recurrence.
MeSH Terms
Figure
Reference
-
1. Martin P. Hepatocellular carcinoma: risk factors and natural history. Liver Transpl Surg. 1998; 4(5 Suppl 1):S87–S91. PMID: 9742499.2. European Association For The Study Of The Liver. European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012; 56:908–943. PMID: 22424438.3. Bruix J, Sherman M. American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011; 53:1020–1022. PMID: 21374666.
Article4. Wang Y, Luo Q, Li Y, Deng S, Wei S, Li X. Radiofrequency ablation versus hepatic resection for small hepatocellular carcinomas: a meta-analysis of randomized and nonrandomized controlled trials. PLoS One. 2014; 9:e84484. PMID: 24404166.
Article5. Makuuchi M, Imamura H, Sugawara Y, Takayama T. Progress in surgical treatment of hepatocellular carcinoma. Oncology. 2002; 62(Suppl 1):74–81. PMID: 11868790.
Article6. Kobayashi M, Ikeda K, Kawamura Y, Yatsuji H, Hosaka T, Sezaki H, et al. High serum des-gamma-carboxy prothrombin level predicts poor prognosis after radiofrequency ablation of hepatocellular carcinoma. Cancer. 2009; 115:571–580. PMID: 19117347.
Article7. Marubashi S, Gotoh K, Akita H, Takahashi H, Ito Y, Yano M, et al. Anatomical versus non-anatomical resection for hepatocellular carcinoma. Br J Surg. 2015; 102:776–784. PMID: 25847111.
Article8. Tomimaru Y, Eguchi H, Marubashi S, Wada H, Kobayashi S, Tanemura M, et al. Equivalent outcomes after anatomical and non-anatomical resection of small hepatocellular carcinoma in patients with preserved liver function. Dig Dis Sci. 2012; 57:1942–1948. PMID: 22407377.
Article9. Yun D, Kim S, Song I, Chun K. Comparative analysis of Laparoscopic versus open surgical radiofrequency ablation for malignant liver tumors. Korean J Hepatobiliary Pancreat Surg. 2014; 18:122–128. PMID: 26155264.
Article10. Livraghi T, Meloni F, Di Stasi M, Rolle E, Solbiati L, Tinelli C, et al. Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: Is resection still the treatment of choice? Hepatology. 2008; 47:82–89. PMID: 18008357.
Article11. Majno PE, Mentha G, Mazzaferro V. Partial hepatectomy versus radiofrequency ablation for hepatocellular carcinoma: confirming the trial that will never be, and some comments on the indications for liver resection. Hepatology. 2010; 51:1116–1118. PMID: 20373366.
Article12. Livraghi T, Meloni F, Morabito A, Vettori C. Multimodal image-guided tailored therapy of early and intermediate hepatocellular carcinoma: long-term survival in the experience of a single radiologic referral center. Liver Transpl. 2004; 10(2 Suppl 1):S98–S106. PMID: 14762848.
Article13. Takayama T, Makuuchi M, Kojiro M, Lauwers GY, Adams RB, Wilson SR, et al. Early hepatocellular carcinoma: pathology, imaging, and therapy. Ann Surg Oncol. 2008; 15:972–978. PMID: 18236118.
Article14. Kagawa T, Koizumi J, Kojima S, Nagata N, Numata M, Watanabe N, et al. Transcatheter arterial chemoembolization plus radiofrequency ablation therapy for early stage hepatocellular carcinoma: comparison with surgical resection. Cancer. 2010; 116:3638–3644. PMID: 20564097.15. Liu Z, Zhou Y, Zhang P, Qin H. Meta-analysis of the therapeutic effect of hepatectomy versus radiofrequency ablation for the treatment of hepatocellular carcinoma. Surg Laparosc Endosc Percutan Tech. 2010; 20:130–140. PMID: 20551807.
Article16. Imai K, Beppu T, Chikamoto A, Doi K, Okabe H, Hayashi H, et al. Comparison between hepatic resection and radiofrequency ablation as first-line treatment for solitary small-sized hepatocellular carcinoma of 3 cm or less. Hepatol Res. 2013; 43:853–864. PMID: 23281579.17. Wang JH, Wang CC, Hung CH, Chen CL, Lu SN. Survival comparison between surgical resection and radiofrequency ablation for patients in BCLC very early/early stage hepatocellular carcinoma. J Hepatol. 2012; 56:412–418. PMID: 21756858.
Article18. Koike Y, Shiratori Y, Sato S, Obi S, Teratani T, Imamura M, et al. Risk factors for recurring hepatocellular carcinoma differ according to infected hepatitis virus-an analysis of 236 consecutive patients with a single lesion. Hepatology. 2000; 32:1216–1223. PMID: 11093727.
Article19. Choi D, Lim HK, Rhim H, Kim YS, Lee WJ, Paik SW, et al. Percutaneous radiofrequency ablation for early-stage hepatocellular carcinoma as a first-line treatment: long-term results and prognostic factors in a large single-institution series. Eur Radiol. 2007; 17:684–692. PMID: 17093964.
Article20. Lam VW, Ng KK, Chok KS, Cheung TT, Yuen J, Tung H, et al. Risk factors and prognostic factors of local recurrence after radiofrequency ablation of hepatocellular carcinoma. J Am Coll Surg. 2008; 207:20–29. PMID: 18589357.
Article21. Lencioni R, Cioni D, Crocetti L, Franchini C, Pina CD, Lera J, et al. Early-stage hepatocellular carcinoma in patients with cirrhosis: long-term results of percutaneous image-guided radiofrequency ablation. Radiology. 2005; 234:961–967. PMID: 15665226.
Article22. Tateishi R, Shiina S, Teratani T, Obi S, Sato S, Koike Y, et al. Percutaneous radiofrequency ablation for hepatocellular carcinoma. An analysis of 1000 cases. Cancer. 2005; 103:1201–1209. PMID: 15690326.23. Guglielmi A, Ruzzenente A, Battocchia A, Tonon A, Fracastoro G, Cordiano C. Radiofrequency ablation of hepatocellular carcinoma in cirrhotic patients. Hepatogastroenterology. 2003; 50:480–484. PMID: 12749252.24. Raut CP, Izzo F, Marra P, Ellis LM, Vauthey JN, Cremona F, et al. Significant long-term survival after radiofrequency ablation of unresectable hepatocellular carcinoma in patients with cirrhosis. Ann Surg Oncol. 2005; 12:616–628. PMID: 15965731.
Article25. Xu HX, Lu MD, Xie XY, Yin XY, Kuang M, Chen JW, et al. Prognostic factors for long-term outcome after percutaneous thermal ablation for hepatocellular carcinoma: a survival analysis of 137 consecutive patients. Clin Radiol. 2005; 60:1018–1025. PMID: 16124984.
Article26. N'Kontchou G, Mahamoudi A, Aout M, Ganne-Carrié N, Grando V, Coderc E, et al. Radiofrequency ablation of hepatocellular carcinoma: long-term results and prognostic factors in 235 Western patients with cirrhosis. Hepatology. 2009; 50:1475–1483. PMID: 19731239.27. Mazzaferro V, Battiston C, Perrone S, Pulvirenti A, Regalia E, Romito R, et al. Radiofrequency ablation of small hepatocellular carcinoma in cirrhotic patients awaiting liver transplantation: a prospective study. Ann Surg. 2004; 240:900–909. PMID: 15492574.28. Iida H, Aihara T, Ikuta S, Yamanaka N. Effectiveness of impedance monitoring during radiofrequency ablation for predicting popping. World J Gastroenterol. 2012; 18:5870–5878. PMID: 23139602.
Article29. Tanaka K, Shimada H, Matsumoto C, Matsuo K, Nagano Y, Endo I, et al. Anatomic versus limited nonanatomic resection for solitary hepatocellular carcinoma. Surgery. 2008; 143:607–615. PMID: 18436008.
Article30. Okamura Y, Ito T, Sugiura T, Mori K, Uesaka K. Anatomic versus nonanatomic hepatectomy for a solitary hepatocellular carcinoma: a case-controlled study with propensity score matching. J Gastrointest Surg. 2014; 18:1994–2002. PMID: 25213582.31. Goh BK, Chow PK, Teo JY, Wong JS, Chan CY, Cheow PC, et al. Number of nodules, Child-Pugh status, margin positivity, and microvascular invasion, but not tumor size, are prognostic factors of survival after liver resection for multifocal hepatocellular carcinoma. J Gastrointest Surg. 2014; 18:1477–1485. PMID: 24855028.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Microwave thermosphere versus radiofrequency ablation for hepatocellular carcinoma: Are we approaching the time to end the debate?
- Surgical resection versus ablation for early hepatocellular carcinoma: The debate is still open
- Radiofrequency Thermal Ablation of Hepatocellular Carcinomas
- Radiofrequency Ablation of Hepatic Cysts: Case Report
- Current status and future of radiofrequency ablation for hepatocellular carcinoma