J Korean Ophthalmol Soc.
2008 Jun;49(6):878-885. 10.3341/jkos.2008.49.6.878.
The Effect of Autologous Dermis-fixation to Orbital Periosteum in Superior Sulcus Deformity
- Affiliations
-
- 1Department of Ophthalmology, Korea University College of Medicine, Seoul, Korea. tsoooo@hanmail.net
- 2Jun Eye Clinic, Seoul, Korea.
- KMID: 2110866
- DOI: http://doi.org/10.3341/jkos.2008.49.6.878
Abstract
-
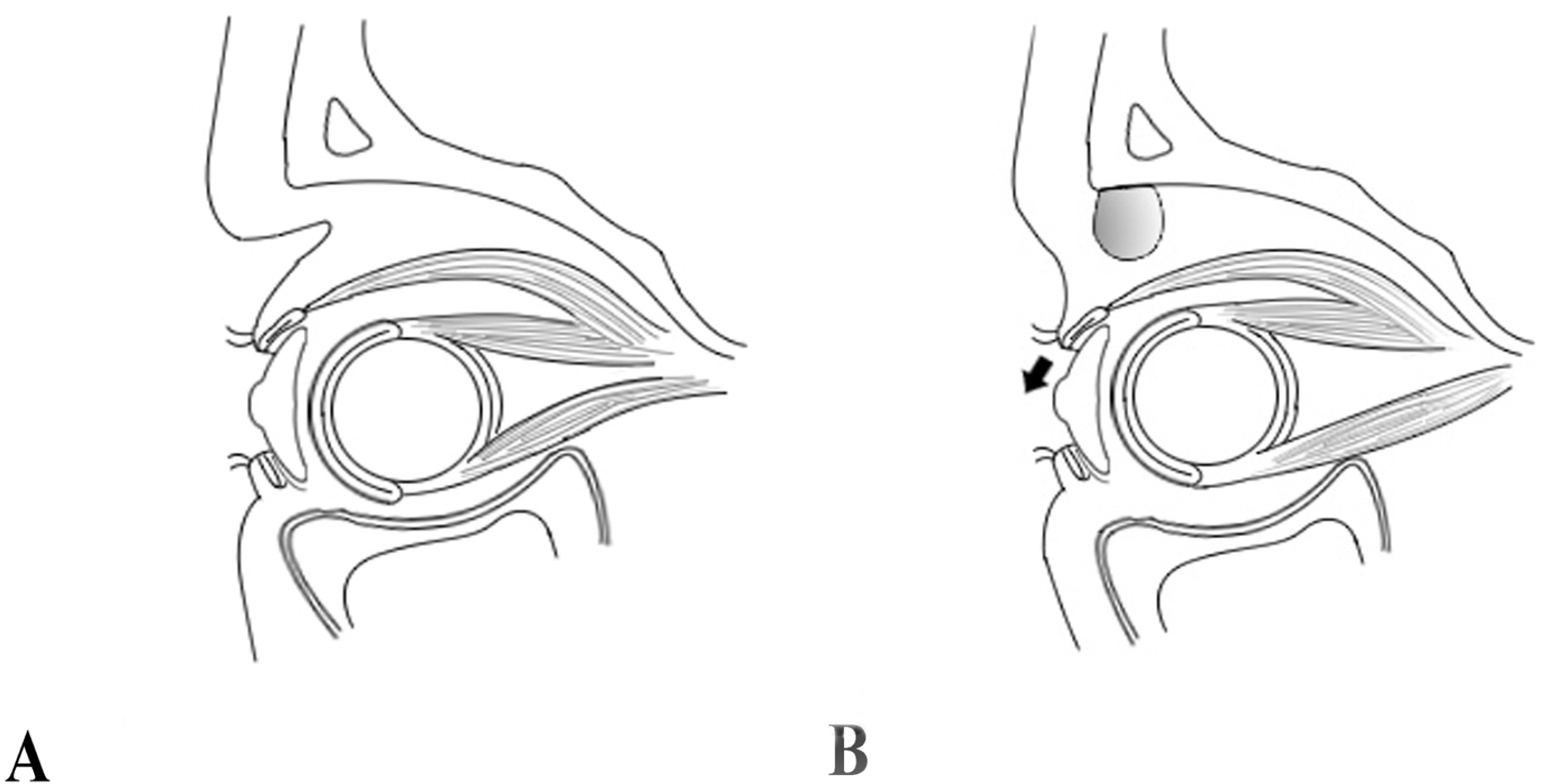
PURPOSE: To evaluate the efficacy of autologus dermis-fixation on the orbital periosteum in patients with superior sulcus deformity.
METHODS
From September 2005 to February 2007, an appropriate amount of a rolled autologus dermis was added to the site of superior sulcus deformity by means of fixation to the orbital periosteum via lid crease incision. Four patients had superior sulcus deformity after undergoing evisceration or other ocular surgeries.
RESULTS
Superior sulcus deformities in all patients could be corrected satisfactorily with bilateral symmetry. During the follow-up period, no complications such as mechanical ptosis and recurrence of superior sulcus deformity were observed.
CONCLUSIONS
The authors believe that autologus dermis-fixation to the orbital periosteum might be a useful method to correct superior sulcus deformity without disturbing movement of the upper eyelid. A study with a larger series of patients and longer follow-up period might be necessary in the future to obtain more information about autologous dermis-fixation to the periosteum in patients with superior sulcus deformity.
Figure
Cited by 1 articles
-
Surgical Outcomes of Levator Resection in Ptosis Patients with Deep Superior Sulcus
Jong Soo Kim, Hee Bae Ahn
J Korean Ophthalmol Soc. 2014;55(12):1734-1738. doi: 10.3341/jkos.2014.55.12.1734.
Reference
-
References
1. Sutula FC, Thomas O. Repair of the superior sulcus deformity using autogenous costal cartilage. Ophthalmology. 1982; 89:424–7.
Article2. Sergott TJ, Vistnes MV. Correction of Enophthalmos and superior sulcus depression in the anophthalmic orbit: A long-term follow-up. Plast Reconstr Surg. 1987; 79:331–8.3. Spivey BE, Allen L, Stewart WB. Surgical correction of superior sulcus deformity occuring after enucleation. Am J Ophthalmol. 1976; 82:365–70.4. Bello VM, Levine MR. Superior sulcus deformity. Arch Ophthalmol. 1980; 98:2215–6.
Article5. Hobar PC, Burt JD, Masson JA. . Pericranial flap correction of superior sulcus depression in the Anophthalmic Orbit. J Craniofac Surg. 1999; 10:487–90.
Article6. Cowen DE, Antonyshyn O. The vascularized temporoparietal fascial flap for correction of the deep superior sulcus. Ophthal Plast Reconstr Surg. 1995; 11:100–8.
Article7. Kim YY, Lee TS. Results of surgical correction for traumatic and anophthalmic enophthalmos. J Korean Ophthalmol Soc. 1988; 29:359–63.8. Iverson RE, Vistnes LM, Siegel RJ. Correction of enophthalmos in the anophthalmic orbit. Plast Reconstr Surg. 1973; 51:545–54.
Article9. Gemert JV, Leone CR. Correction of a deep superior sulcus with dermis‐ fat implantation. Arch Ophthalmol. 1986; 104:640–7.10. Sihota R, Sujatha Y, Betharia SM. The fat pad in dermis fat grafts. Ophthalmology. 1994; 101:231–4.
Article11. Lee Y, Kwon S, Hwang K. Correction of sunken and/or multiple folded upper eyelid by fascia-fat graft. Plast Reconstr Surg. 2001; 107:15–9.12. Smith B, Lisman RD. Use of sclera and liquid collagen in the camouflage of superior sulcus deformities. Ophthalmology. 1983; 90:230–235.
Article13. Laiseca A, Laiseca D, Laiseca J. Laiseca J Jr. Correcting superior sulcus deformities. Adv Ophthalmol Plast Reconstr Surg. 1990; 8:229–33.14. Taiara C, Smith B. Correction of enophthalmos and supratarsal sulcus by posterior subosteal glass bead implantation. Br J Ophthalmol. 1973; 57:741–4.15. Sclafani AP. . Homologous collagen dispersion (Dermalogen) as a dermal filler: Persistence and histology compared with bovine collagen. Ann Plast Surg. 2002; 49:181–8.
Article16. Sclafani AP. Romo T III. Collagen, human collagen, and fat:The search for a three‐ Dimensional soft tissue filler. Facial Plast Surg. 2001; 17:79–85.17. Pollack S. Some new injectable dermal filler materials : Hylaform, Restylane, and Artecoll. J Cutan Med Surg. 1999; 3:S27-35.18. Naoum C. Dasiou-Plakida D. Dermal filler materials and Botulinum toxin. Int J Derm. 2001; 40:609–21.19. Fagien S. Facial soft‐ tissue augmentation with injectable autologous and allogeneic human tissue collagen matrix (Autologen and Dermalogen). Plast Reconstr Surg. 2000; 105:362–73.20. Alster TS, West TB. Human‐ derived and new synthetic injectable materials for soft‐ tissue augmentation: Current status and role in cosmetic surgery. Plast Reconstr Surg. 2000; 105:2515–25.21. Stegman SJ, Chu S, Armstrong RC. Adverse reactions to bovine collagen implant: clinical and histological features. J Dermatol Surg Oncol. 1988; 14:3948.22. Devoe AG. Experiences with the surgery of the anophthalmic orbit. Am J Ophthalmol. 1945; 28:1346–51.
Article23. Vistnes LM. Mechanism of upper lid ptosis in the anophthalmic orbit. Plast Reconstr Surg. 1976; 58:539–45.
Article24. Tyers AC, Collin JR. Orbital implants and post enucleation socket syndrome. Trans Ophthalmol Soc U K. 1982; 102:90–2.25. Smit TJ, Koornneef L, Zonneveld FW. . Computed tomography in the assessment of the postenucleation socket syndrome. Ophthalmology. 1990; 97:1347–51.
Article26. Reed RK, Laurent UB, Frazer JR, Laurent TC. Removal rate of [3H] hyaluronan injected subcutaneously in rabbits. Am J Physiol. 1990; 259:532–5.27. Duranti F, Salti G, Bovani B. . Injectable hyaluronic acidgel for soft tissue augmentation A clinical and histological study. Dermatol Surg. 1998; 24:1317–25.28. Latouche X, Illouz Y. The value of a new filler material in corrective and cosmetic surgery: Derma Liveand Derma Deep. Aesth Plast Surg. 2001; 25:249–55.29. Schanz S, Schippert W, Ulmer A. . Arterial embolization caused by injection of hyaluronic acid (Restylane). Br J Dermatol. 2002; 146:928–9.30. Rubin PA, Fay AM, Remulla HD, Maus M. Ophthalmic plastic applications of acellular dermal grafts. Ophthalmology. 1999; 106:2091–7.31. Sullivan SA, Dailey RA. Graft contraction of acellular dermis versus hard palate mucosa in lower eyelid surgery. Ophthal Plast Reconstr Surg. 2003; 19:14–24.32. Mauriello JA, Fiore PM, Pokorny KS, Cinotti DJ. Use of split-thickness dermal graft in the surgical treatment of corneal and scleral defects. Am J Ophthalmol. 1988; 105:244–7.
Article33. Mauriello JA, Han KH, Wolfe R. Use of autogenous split‐ thickness dermal graft for reconstruction of the lining of the exentrated orbit. Am J Ophthalmol. 1985; 100:465–7.34. Shore JW, McCord CD, Bergin DJ. . Management of complications following dermis‐ fat grafting for anophthalmic socket reconstruction. Ophthalmology. 1985; 92:1342–50.35. Wojno T, Tenzel R. Dermis grafts in socket reconstruction. Ophthalmic Plast Reconstr Surg. 1985; 2:7–14.
Article36. Cannada JE. Some uses of the cutis graft in surgery. Am J Surg. 1943; 59:409–19.37. Park MS, Kim KS, Baek SH, Lee TS. Management of exposed porous orbital implant with autogenous dermis graft. J Korean Ophthalmol Soc. 2001; 42:1127–32.38. Thomson N. The subcuteneous dermis graft: a clinical and histologic study n man. Plast Reconstr Surg. 1960; 26:1–22.39. Peer LA, Paddock R. Histologic studies on the fate of deeply implanted dermal graft: observations on sections of implanted buried from one week to one year. Arch Surg. 1937; 34:268–90.40. Georgiade NG, Altany F, Pickrell K. An experimental and clinical evaluation of autogenous dermal grafts used in the treatment of temporomandibular joint ankylosis. Plast Reconstr Surg. 1957; 19:321–36.
Article41. Erdogan B, Tuncel A, Adanali G. Augmentation rhinoplasty with dermal graft and review of the literature. Plast Reconstr Surg. 2004; 113:1080–91.
Article42. Mackay DR, Manders EK, Suggers GC. The fate of dermal and dermal-fat graft. Ann Plast Surg. 1993; 31:42–6.43. Sevin BA, Adanali G, Yakut M. . The fate of folded and unfolded dermal grafts: A histopatholotic and structural study of rabbits. Aesthetic Plast Surg. 2006; 30:486–91.44. Khan JA, Dermal graft. Alternative to Gunderson flap allows scleral shell over sensitive cornea. Ophthal Plast Reconstr Surg. 1990; 6:260–4.45. Dimitroulis G. The use of dermis graft after discectomy for internal derangement of the temporomandibular joint. J Oral Maxillofac Surg. 2005; 63:173–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Perlane(R) Injection on Superior Sulcus Deformity
- Clinical Efficacy of Dermis-Fat Graft vs. Posterior Tenon's Capsule Suturing in Anophthalmic Orbit
- Correction of Superior Sulcus Deformity and Enophthalmos with Porous High-density Polyethylene Sheet in Anophthalmic Patients
- Outcomes of Autogenous Dermis Fat Grafting with Different Donor Sites in Exposed Porous Orbital Implants
- The Use of Mesh Microplates in Management of Comminuted Nasal Bone Fracture