J Korean Orthop Assoc.
2008 Apr;43(2):152-159. 10.4055/jkoa.2008.43.2.152.
Clinical Efficacy of a Stand-Alone, Threaded-Titanium Fusion Cage for Single-Level Degenerative Lumbar Spinal Disorders
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Research Institute of Clinical Medicine,Chonbuk National University Hospital, Korea. kysong@chonbuk.ac.kr
- 2Department of Orthopedic Surgery, Gwangju Veterans Hospita, Korea.
- 3Department of Orthopedic Surgery, Jeju National University Hospital, Korea.
- KMID: 2106433
- DOI: http://doi.org/10.4055/jkoa.2008.43.2.152
Abstract
-
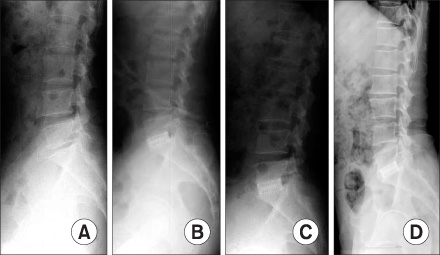
PURPOSE: To evaluate the clinical and radiologic efficacy of posterior lumbar interbody fusion (PLIF) using a threaded fusion cage (TFC) alone with autogenous iliac corticocancellous bone graft for single-level degenerative lumbar spinal disorders.
MATERIALS AND METHODS
Thirty-eight consecutive patients receiving PLIF with TFC alone were evaluated with at least three years of follow-up. Clinical outcome and satisfaction were assessed using Ragab's measurements. Radiological outcomes were analyzed in terms of lumbar lordosis, segmental lordosis, disc height, and fusion rates.
RESULTS
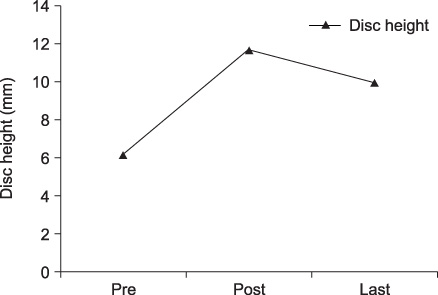
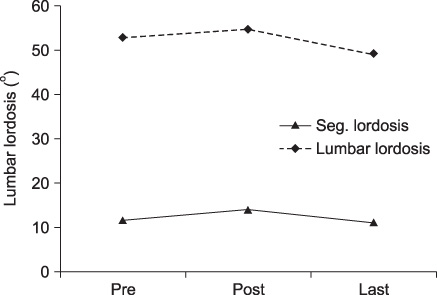
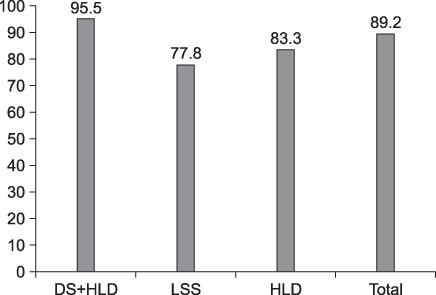
Disc height was 6.18+/-2.54 mm, 11.71+/-1.60 mm and 9.94+/-1.94 mm on average for preoperative, postoperative, and final follow-up, respectively. Lumbar lordosis was 27.46+/-11.47degrees, 31.41+/-8.89degrees on average for preoperative and at final follow-up, respectively. Segmental lordosis was 11.51+/-9.35degrees preoperatively, and 10.86+/-7.49degrees at final follow-up. Satisfactory clinical outcome were obtained in 89.2% of patients with successful bone fusion in 73.0% of patients.
CONCLUSION
Stand alone TFC is an effective treatment modality in maintenance of disc height and lumbar lordosis, with satisfactory long term clinical outcomes in the treatment of single-level degenerative lumbar spinal disorders.
Keyword
Figure
Cited by 3 articles
-
Lumbar Lordosis Restoration with an Eight Degree Cage in Posterior Lumbar Interbody Fusion for Lumbar Degenerative Disease
Young-Tae Kim, Kyu-Jung Cho, Ju-Yong Park, Jong-Hyuk Yang
J Korean Orthop Assoc. 2014;49(3):177-184. doi: 10.4055/jkoa.2014.49.3.177.Restoration of Lumbar Lordosis After Posterior Lumbar Interbody Fusion with 4 Degree Cage in Degenerative Spinal Disease
Kyu-Jung Cho, Young-Tae Kim, Seung-Rim Park, Seung-Hyun Hong
J Korean Soc Spine Surg. 2013;20(2):51-57. doi: 10.4184/jkss.2013.20.2.51.Restoration of Segmental Lordosis and Related Factors in Interbody Fusion for Degenerative Lumbar Disease
Eung-Ha Kim, Jung-Moo Seo, Joong-Hyeon Ahn
J Korean Soc Spine Surg. 2015;22(4):170-177. doi: 10.4184/jkss.2015.22.4.170.
Reference
-
1. Agazzi S, Reverdin A, May D. Posterior lumbar interbody fusion with cages. An independent review of 71 cases. J Neurosurg. 1999. 91:Suppl 2. S186–S192.
Article2. Ahn JS, Lee JK, Yang JY, Kim YM, Kim SB, Lee MJ. Relationship between union of grafted autologous bone and clinical results of operative treatment of degenerative spondylolisthesis by posterolateral fusion. J Korean Orthop Assoc. 1999. 34:95–101.
Article3. Bagby GW. Arthrodesis by the distraction-compression method using a stainless steel implant. Orthopedics. 2003. 6:931–934.
Article4. Blumenthal SL, Ohnmeiss DD. NASS. Intervertebral cages for degenerative spinal disease. Spine J. 2003. 3:301–309.5. Cho JL, Park YS, Han JH, Lee CH, Roh WI. The change of adjacent segments after spinal fusion. J Korean Spine Surg. 1998. 5:239–246.6. Cloward RB. The treatment of ruptured lumbar intervertebral discs by vertebral body fusion. I. Indications, operative technique, after care. J Neurosurg. 1953. 10:154–168.7. Dick W. The fixateur interne as a versatile implant for spine surgery. Spine. 1987. 12:882–900.8. Elias WJ, Simmons NE, Kaptain GJ, Chadduck JB, Whitehill R. Complications of posterior lumbar interbody fusion when using a titamium threaded cage devices. J Neurosurg. 2000. 93:Suppl 1. S45–S52.9. Evans JH. Biomechanics of lumbar fusion. Clin Orthop Relat Res. 1985. 193:38–46.
Article10. Fuji T, Oda T, Kato Y, Fujita S, Tanaka M. Posterior lumbar interbody fusion using titanium cylindrical threaded cages: is optimal interbody fusion possible without other instrumentation? J Orthop Sci. 2003. 8:142–147.
Article11. Hutter CG. Posterior intervertebral body fusion. A 25-year study. Clin Orthop Relat Res. 1983. 179:86–89.
Article12. Lang P, Genant HK, Chafetz N, Steiger P, Morris JM. Three-dimensional computed tomography and multiplanar reformations in the assessment of pseudoarthrosis in posterior lumbar interbody fusion patients. Spine. 1988. 13:69–75.13. Lin PM, Cautilli RA, Joyce MF. Posterior lumbar interbody fusion. Clin Orthop Relat Res. 1983. 180:154–168.
Article14. Lin PM. Posterior lumbar interbody fusion technique: complications and pitfalls. Clin Orthop Relat Res. 1985. 193:90–102.15. Ma GW. Posterior lumbar interbody fusion with specialized instruments. Clin Orthop Relat Res. 1985. 193:57–63.
Article16. McAfee PC. Interbody fusion cage in reconstructive operation on the spine. J Bone Joint Surg Am. 1999. 81:859–880.17. Mosdal C. Cervical osteochondrosis and disc herniation. Eighteen years' use of interbody fusion by Cloward's technique in 755 cases. Acta Neurochirurgica (Wien). 1985. 70:207–225.
Article18. Otero Vich JM. Anterior cervical interbody fusion with threaded cylindrical bone. J Neurosurg. 1985. 63:750–753.
Article19. Park HK, Rha HK, Lee GS, Choi CR, Song JU, Ahn MS. Surgical treatment of lumbar spondylolisthesis. J Korean Neurosurg Soc. 1989. 18:613–621.20. Ragab AA, Fye MA, Bohlman HH. Surgery of the lumbar spine for spinal stenosis in 118 patients 70 years of age or older. Spine. 2003. 28:348–353.
Article21. Ray CD. Threaded fusion cages for lumber intebody fusions. Spine. 1997. 22:667–680.22. Ray CD. Threaded titanium cages for lumbar interbody fusions. An economic comparison with 360 degree fusion. Spine. 1997. 22:681–685.23. Ricciardi JE, Pflueger PC, Isaza JE, Whitecloudll TS 3rd. Transpedicular fixation for the treatment of isthmic spondylolisthesis in adults. Spine. 1995. 20:1917–1922.
Article24. Roy-Camille R. Osteogynthese du rachis dorsal, lumbar, and lumbosacral spine with metallic plates screwed into vertebral pedicles and articular apophyses. Presse Med. 1970. 78:1447–1448.25. Song KJ, Kim SJ. Surgical treatment for the low grade lumbar isthmic spondylolithesis: comparison between post-erolateral fusion and posterior lumbar interbody fusion. J Kor Soc Spine Surg. 1999. 6:96–103.26. Tullberg T, Brandt B, Rydgerg J, Fritzell P. Fusion rate after posterior lumbar interbody fusion with carbon fiber implant: 1-year follow-up of 51 patients. Eur Spine J. 1996. 5:178–182.
Article27. Wetzel FT, LaRocca H. The failed posterior lumbar interbody fusion. Spine. 1991. 16:839–845.
Article28. Wiltse LL, Newman PH, Macnab I. Classification of spondylolysis and spondylolisthes. Clin Orthop Relat Res. 1976. 117:23–29.29. Yi HJ, Kim NK, Lee SR, et al. Clinical, radiological analysis of TFC in surgical treatment of spondylolisthesis. J Korean Neurosurg Soc. 1995. 24:766–775.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posterior Lumbar Interbody Fusion with Threaded Fusion Cage(TFC)
- Posterior Lumbar Interbody Fusion with Threaded Fusion Cage: Long-term Follow-up Results
- Anterior Cervical Bisegmental Interbody Fusion with Titanium Cage(RABEA) in Degenerative Cervical Disease: Comparative Analysis with Monosegmental Interbody Fusion
- Results of Four-Level Anterior Cervical Discectomy and Fusion Using Stand-Alone Interbody Titanium Cages
- The Advantages of Rectangular Titanium Cage(RABEA) Fusion after Anterior Cervical Discectomy: Comparative Study of Fibula Allograft