J Korean Soc Spine Surg.
2004 Jun;11(2):104-112. 10.4184/jkss.2004.11.2.104.
The Effect of Shoe Lift on Lumbar Scoliosis Associated with Pelvic Obliquity
- Affiliations
-
- 1Department of Orthopedic Surgery, Chungbuk National University Hospital, Cheongju, Korea. ymkim@med.chungbuk.ac.kr
- KMID: 2097817
- DOI: http://doi.org/10.4184/jkss.2004.11.2.104
Abstract
- STUDY DESIGN: A retrospective study designed to evaluate the effect of a shoe lift on the lumbar scoliosis associated with pelvic obliquity.
OBJECTIVES
To analyze the changes in pelvic height, Cobb angle and clinical manifestations after application of a shoe lift. SUMMARY OF LITERATURE REVIEW: The most common form of scoliosis in adolescence is idiopathic (85% of scoliosis), which is a form of structural scoliosis. Some non-structural scoliosis may be assessed as an idiopathic form, which can result in an unnecessary treatment, such as bracing. Pelvic obliquity may be a cause of non-structural scoliosis, and a shoe lift may be used for its correction.
MATERIALS AND METHODS
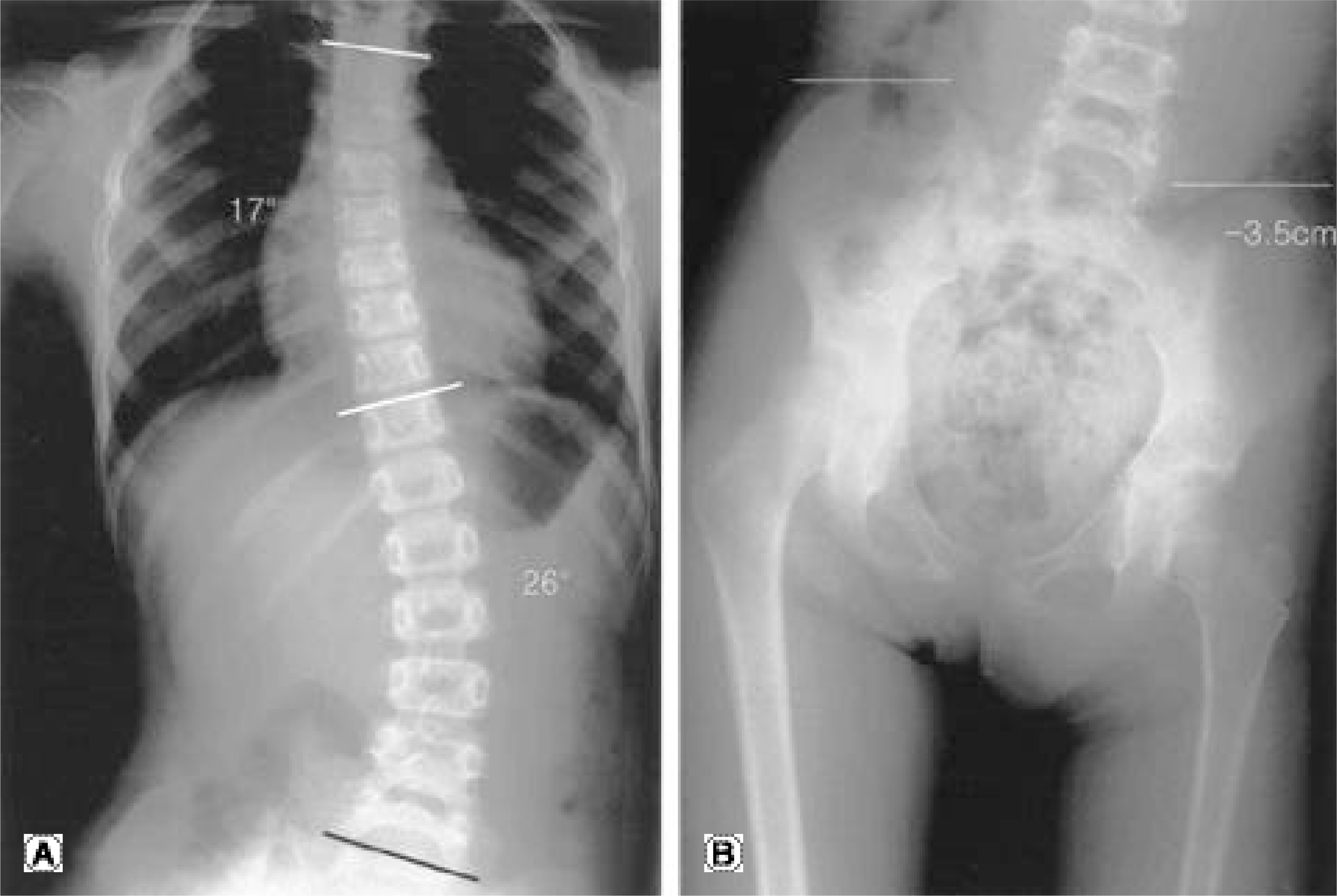
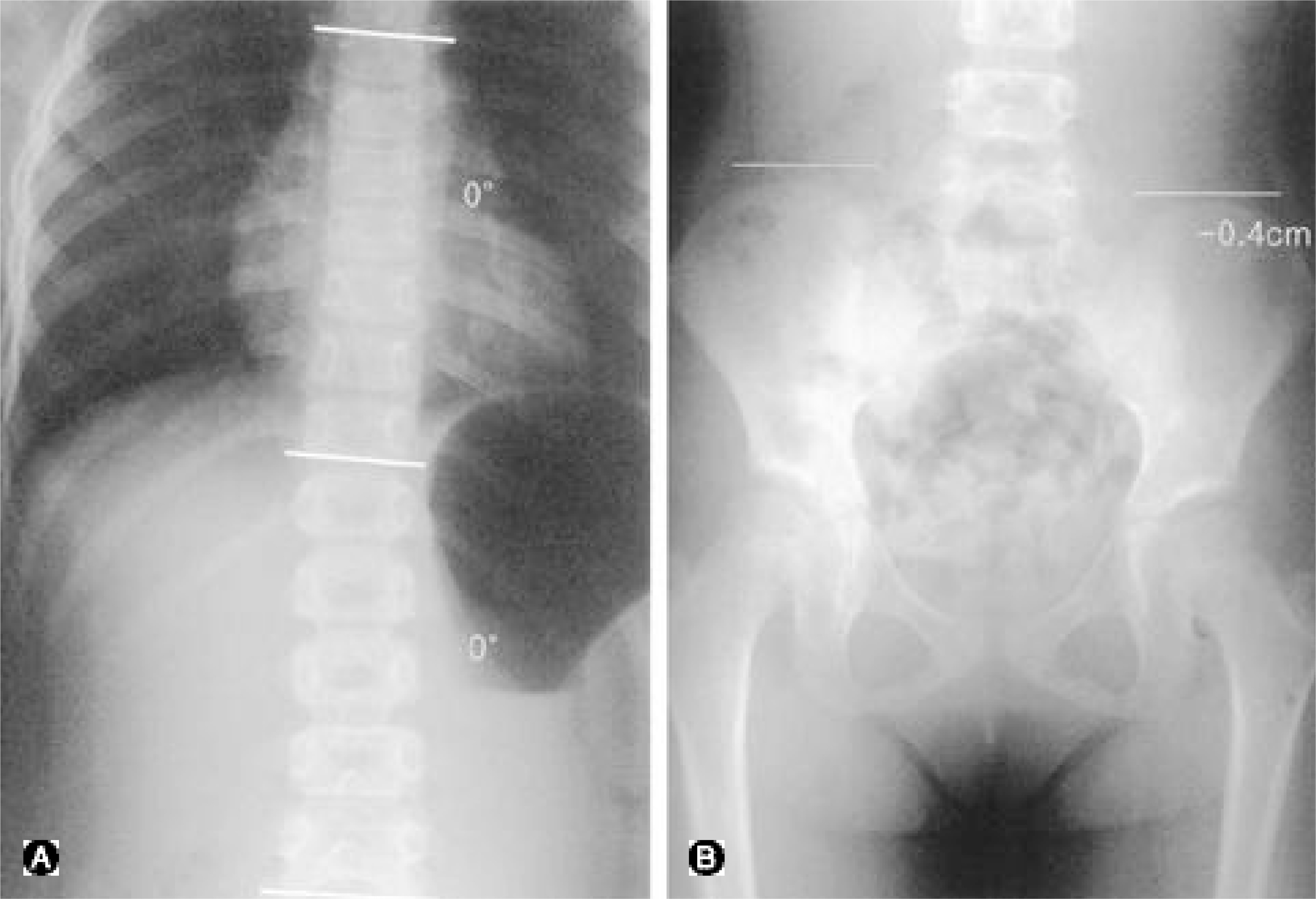
Twelve cases of lumbar scoliosis associated with pelvic obliquity, between April, 1998 and October, 2002, were investigated for the changes in the pelvic height and Cobb angle. Standing T-L AP and standing pelvic AP for measuring the Cobb angle and pelvic obliquity, respectively, were checked before and after application of a shoe lift. The Bell-Thompson method was used for measuring the limb length discrepancy. The shoe lift was composed of a compact cork pad and soft sponge tissue. The extent of a shoe lift was determined with the use of the most comfortable wood block height on stand-ing still. The radiological and clinical outcomes of the shoe lift were investigated.
RESULTS
After the introduction of the shoe lift, 9 cases (75%) achieved a leveled pelvis (height difference less than 0.3cm) 1 week post-shoe lift. The mean Cobb angle before treatment was 16degrees ranging from 9 to 26degrees which was reduced to 6.7degrees ranging from 0 to 23degrees due to the shoe lift 1 week post-shoe lift. The mean correction of the Cobb angle after the introduction of a shoe lift was 73.9%. Clinically, 2 cases with low back pain achieved an improvement in the pain, and most patients expressed that walk-ing and standing had become more comfortable.
CONCLUSION
A shoe lift seems to be significantly effective in correcting the Cobb angle and pelvic height in lumbar scoliosis associated with pelvic obliquity.
Keyword
MeSH Terms
Figure
Reference
-
1). Giles LGF and Taylor JR. Lumbar spine structural change associated with leg length inequality. Spine. 1982; 7:159–162.2). Apley A. System of Orthopaedics and Fractures. 5th ed.London: Butterworths;p. 25–209. 1977.3). James JIP. Scoliosis. 2nd edition.Edinburgh: Churchill Livingstone;1976.4). Wiels P and Sweetmann R. Compensatory lateral curvature. Essentials of Orthopedics London. J & A Chur chill:. 16-17:1965.5). Zabjek KF, Leroux MA, Coillard C, et al. Acute postur -al adaptation induced by a shoe lift in idiopathic scoliosis patients. Eur Spine J. 2001; 10:107–113.6). Cyriax J. Texbook of Orthopaedic Medicine. Vol. 1. 5th edition.London, Cassell & Co: 442;1969.7). Giles LGF. Leg length inequalities associated with low back pain. JCCA. 1976; 20:25–32.8). Sicuranza Bj, Richards J and Tisdall LH. The short leg syndrome in obstetrics and gynecology. Am J Obstet Gynecol. 1970; 107:217–217.
Article9). Stoddard A. Manual of Osteopedic Technique. London: Hutchinson Medical Publications;p. 212. 1959.10). Yates A. The lumbar spine and back pain. Treatment of Back Pain. M Jayson, editor. London: Sector Publishing Ltd;p. 341–353. 1976.11). William D, Bandy WD and Sinning WE. Ki ne matic effects of heel lift use to correct lower limb length difference. Journal of Orthopedic and Sports Physical Therapy. 1986; 7:173–179.12). Gibson PH, Papaioannou T and Kenwright J. T h e influence of the spine of leg length discrepancy after femoral fracture. J Bone Joint Surg. 1983; 65-B:584–587.13). Papaioannou T, Stroke I and Kenwright J. Sc oliosis associated limb length inequality. J Bone Joint Surg. 1982; 64-A:59–61.14). Bourdillon JF. Spinal Manipulation. London: William Heinemann Medical Books Ltd;1970.15). Nichols PJR. Short-leg syndrome. Br Med J. 1960; 1863-1865.
Article16). Rush WA and Steiner HA. A study of lower extremity length inequality. Am J Roentgen. 1946; 56:616–623.17). Steven M. Blustein and Joseph C. D’ Amico. Limb length discrepancy. J Am Podiatr Med Assoc. 1985; 4:200–206.18). Cummings G, Scholz MS and Barnes K. The effect of imposed leg length difference on pelvic bone symmetry. Spine. 1993; 18:368–373.
Article19). Gofton JP. Studies in osteoarthritis of the hip. Biome -chanics and clinical considerations. Can Med Assoc J. 1971; 104:1007.20). Giles LGF and Taylor JR. Low back pain associated with leg length inequlity. Spine. 1981; 6:510–521.21). Walker AP and Dickinson RA. School screening and pelvic tilt scoliosis. Lancet. 1984; 21:152–154.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Attenuation of Spinal Curvature and Pelvic Obliquity by Body Shape Molded Inner System in Cerebral Palsy with Non-Fixed Scoliosis
- The Role of Lumbodorsal Fascotomy in the Treatment of Peratlytic Scoliosis and Pelvic Obliquity
- Association between Sacral Slanting and Adjacent Structures in Patients with Adolescent Idiopathic Scoliosis
- The Treatment of Fixed Pelvic Obliquity in Paralytic Scoliosis
- Classification and Management of Fixed Paralytic Pelvic Obliquity