Korean J Hematol.
2012 Jun;47(2):136-141. 10.5045/kjh.2012.47.2.136.
Changes in hematologic indices in caucasian and non-caucasian pregnant women in the United States
- Affiliations
-
- 1Department of Pathology, University of Pittsburgh Medical Center, University of Pittsburgh, PA, USA.
- 2The Institute for Transfusion Medicine, University of Pittsburgh, PA, USA.
- 3Department of Anesthesiology, Magee Womens Hospital of the University of Pittsburgh Medical Center, University of Pittsburgh, PA, USA. watejh@upmc.edu
- 4Department of Bioengineering, University of Pittsburgh, PA, USA.
- KMID: 2083608
- DOI: http://doi.org/10.5045/kjh.2012.47.2.136
Abstract
- BACKGROUND
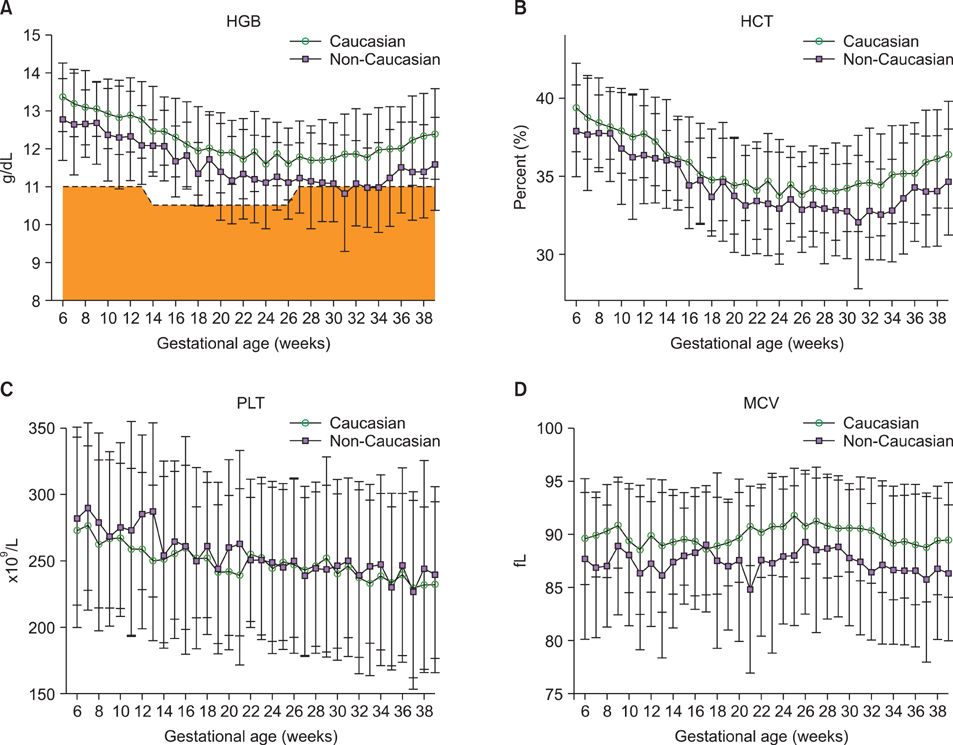
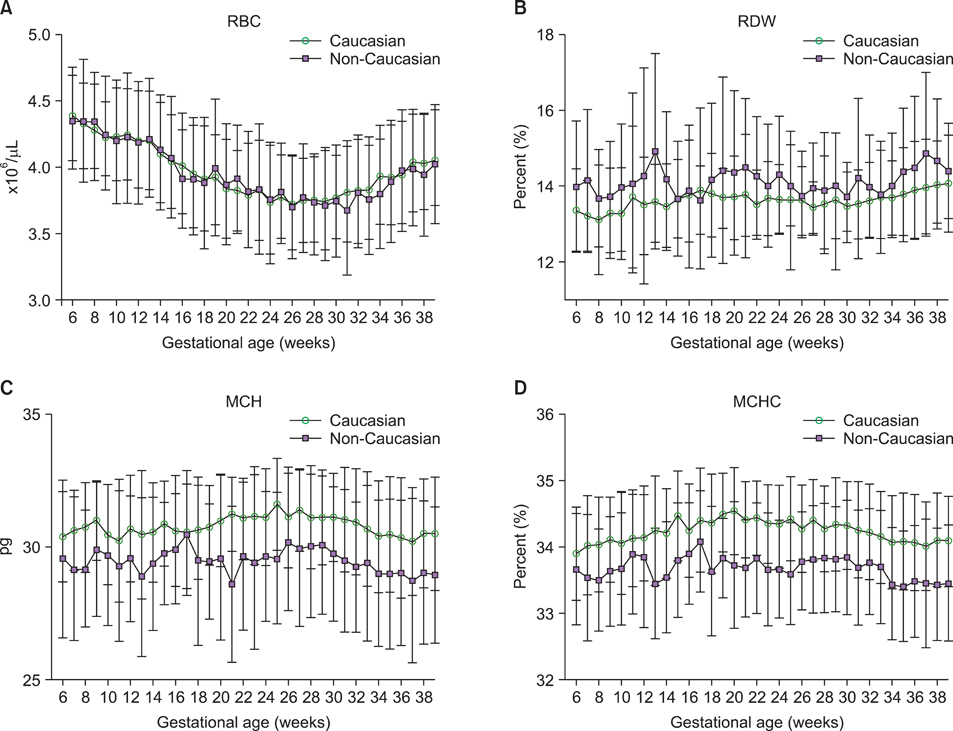
The objective of this study was to determine if there are differences in common red blood cell (RBC) indices and platelet concentrations during pregnancy and to establish if any observed differences in these parameters were based on the patient's ethnicity.
METHODS
From an electronic perinatal database which stores laboratory and clinical information on a large number of births at a regional hospital specializing in obstetrical care, RBC index and platelet concentration data were retrospectively analyzed at various time points throughout pregnancy. RBC index data was collected from 8,277 pregnant women (5,802 Caucasian pregnant women and 2,475 non-Caucasian pregnant women). Platelet concentration data was available from 8252 pregnant women (5,784 Caucasian pregnant women and 2,468 non-Caucasian pregnant women).
RESULTS
Hemoglobin (HGB) levels were significantly higher amongst Caucasian women compared to non-Caucasian women (P at least <0.01) starting at 27 weeks gestation and proceeding until term. There was no significant difference in the mean PLT counts between Caucasian and non-Caucasian pregnant women at any point during gestation.
CONCLUSION
There are ethnic differences in HGB levels, but not the platelet concentrations, during pregnancy. Based on this finding it would be reasonable to conduct formal prospective studies to determine the clinical significance of this difference and to establish the threshold for diagnosing gestational anemia, especially in pregnant non-Caucasian women.
Keyword
MeSH Terms
Figure
Reference
-
1. Sifakis S, Pharmakides G. Anemia in pregnancy. Ann N Y Acad Sci. 2000. 900:125–136.
Article2. Lund CJ, Donovan JC. Blood volume during pregnancy. Significance of plasma and red cell volumes. Am J Obstet Gynecol. 1967. 98:394–403.3. Centers for Disease Control and Prevention. Recommendations to prevent and control iron deficiency in the United States. MMWR Recomm Rep. 1998. 47:1–29.4. Svanberg B, Arvidsson B, Norrby A, Rybo G, Sölvell L. Absorption of supplemental iron during pregnancy - a longitudinal study with repeated bone-marrow studies and absorption measurements. Acta Obstet Gynecol Scand Suppl. 1975. 48:87–108.5. Sjostedt JE, Manner P, Nummi S, Ekenved G. Oral iron prophylaxis during pregnancy: a comparative study on different dosage regimens. Acta Obstet Gynecol Scand Suppl. 1977. 60:3–9.6. Taylor DJ, Mallen C, McDougall N, Lind T. Effect of iron supplementation on serum ferritin levels during and after pregnancy. Br J Obstet Gynaecol. 1982. 89:1011–1017.
Article7. Puolakka J, Jänne O, Pakarinen A, Järvinen PA, Vihko R. Serum ferritin as a measure of iron stores during and after normal pregnancy with and without iron supplements. Acta Obstet Gynecol Scand Suppl. 1980. 95:43–51.
Article8. Milman N, Bergholt T, Byg KE, Eriksen L, Hvas AM. Reference intervals for haematological variables during normal pregnancy and postpartum in 434 healthy Danish women. Eur J Haematol. 2007. 79:39–46.
Article9. Kaneshige E. Serum ferritin as an assessment of iron stores and other hematologic parameters during pregnancy. Obstet Gynecol. 1981. 57:238–242.10. James TR, Reid HL, Mullings AM. Are published standards for haematological indices in pregnancy applicable across populations: an evaluation in healthy pregnant Jamaican women. BMC Pregnancy Childbirth. 2008. 8:8.
Article11. Johnson-Spear MA, Yip R. Hemoglobin difference between black and white women with comparable iron status: justification for race-specific anemia criteria. Am J Clin Nutr. 1994. 60:117–121.
Article12. Perry GS, Byers T, Yip R, Margen S. Iron nutrition does not account for the hemoglobin differences between blacks and whites. J Nutr. 1992. 122:1417–1424.
Article13. Hellgren M. Hemostasis during normal pregnancy and puerperium. Semin Thromb Hemost. 2003. 29:125–130.
Article14. American College of Obstetricians and Gynecologists. ACOG practice bulletin: Thrombocytopenia in pregnancy. Number 6, September 1999. Clinical management guidelines for obstetrician-gynecologists. Int J Gynaecol Obstet. 1999. 67:117–128.15. Burrows RF, Kelton JG. Incidentally detected thrombocytopenia in healthy mothers and their infants. N Engl J Med. 1988. 319:142–145.
Article16. Burrows RF, Kelton JG. Thrombocytopenia at delivery: a prospective survey of 6715 deliveries. Am J Obstet Gynecol. 1990. 162:731–734.
Article17. Samuels P, Bussel JB, Braitman LE, et al. Estimation of the risk of thrombocytopenia in the offspring of pregnant women with presumed immune thrombocytopenic purpura. N Engl J Med. 1990. 323:229–235.
Article18. Aster RH. "Gestational" thrombocytopenia: a plea for conservative management. N Engl J Med. 1990. 323:264–266.19. Hart D, Dunetz C, Nardi M, Porges RF, Weiss A, Karpatkin M. An epidemic of maternal thrombocytopenia associated with elevated antiplatelet antibody. Platelet count and antiplatelet antibody in 116 consecutive pregnancies: relationship to neonatal platelet count. Am J Obstet Gynecol. 1986. 154:878–883.
Article20. Romslo I, Haram K, Sagen N, Augensen K. Iron requirement in normal pregnancy as assessed by serum ferritin, serum transferrin saturation and erythrocyte protoporphyrin determinations. Br J Obstet Gynaecol. 1983. 90:101–107.
Article21. State & County Quickfacts. US Census Bureau. Accessed December 6, 2011. Suitland, MD: US Census Bureau;at http://quickfacts.census.gov/qfd/states/42/42003.html.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Neonatal and Infant Mortality Rates between Infants Born in South Korea and Those Born in the United States
- The Influence of Culture on the Experiences of Korean, Korean American, and Caucasian-American Family Caregivers of Frail Older Adults: A Literature Review
- Facial form analysis of the lower and middle face in young Korean women
- A Study on the Climacteric Symptoms and Emotion of Korean Women Living in the United States and Korea
- A case of angioedema associated with eosinophilia