Korean J Radiol.
2014 Jun;15(3):334-345. 10.3348/kjr.2014.15.3.334.
CT Findings of Gallbladder Metastases: Emphasis on Differences According to Primary Tumors
- Affiliations
-
- 1Department of Radiology, Seoul National University Hospital, Seoul 110-744, Korea. shkim7071@gmail.com
- 2Department of Pathology, Seoul National University Hospital, Seoul 110-744, Korea.
- 3Department of Internal Medicine, Inje University Seoul Paik Hospital, Inje University College of Medicine, Seoul 100-032, Korea.
- KMID: 2078643
- DOI: http://doi.org/10.3348/kjr.2014.15.3.334
Abstract
OBJECTIVE
To describe computed tomography (CT) features of metastatic gallbladder (GB) tumors (MGTs) from various primary tumors and to determine whether there are differential imaging features of MGTs according to different primary tumors.
MATERIALS AND METHODS
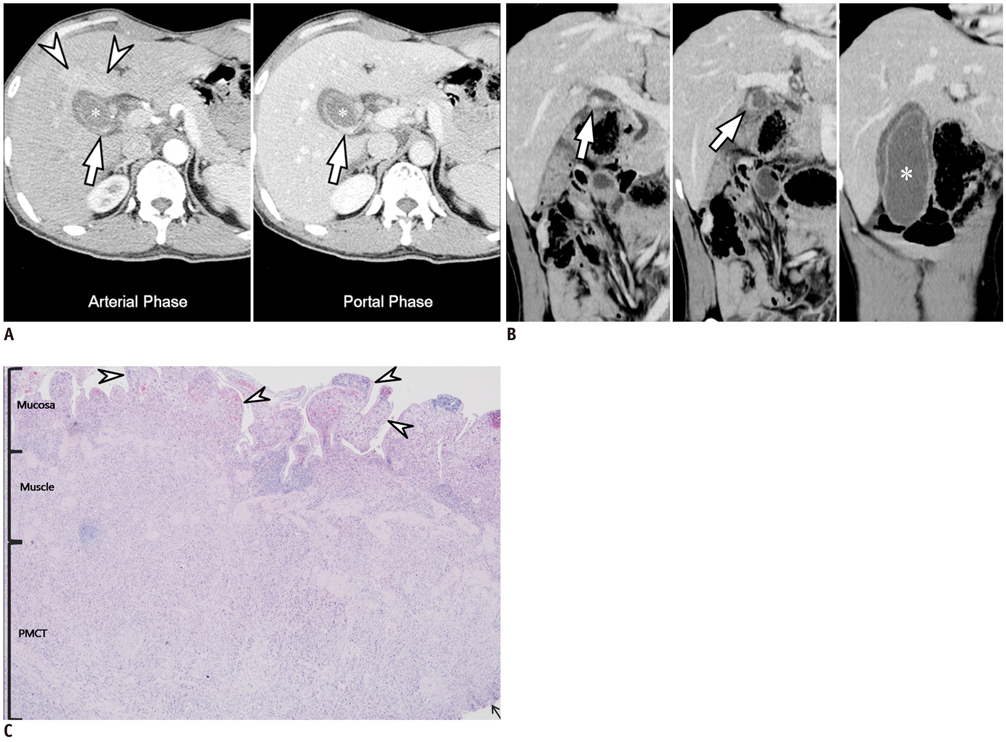
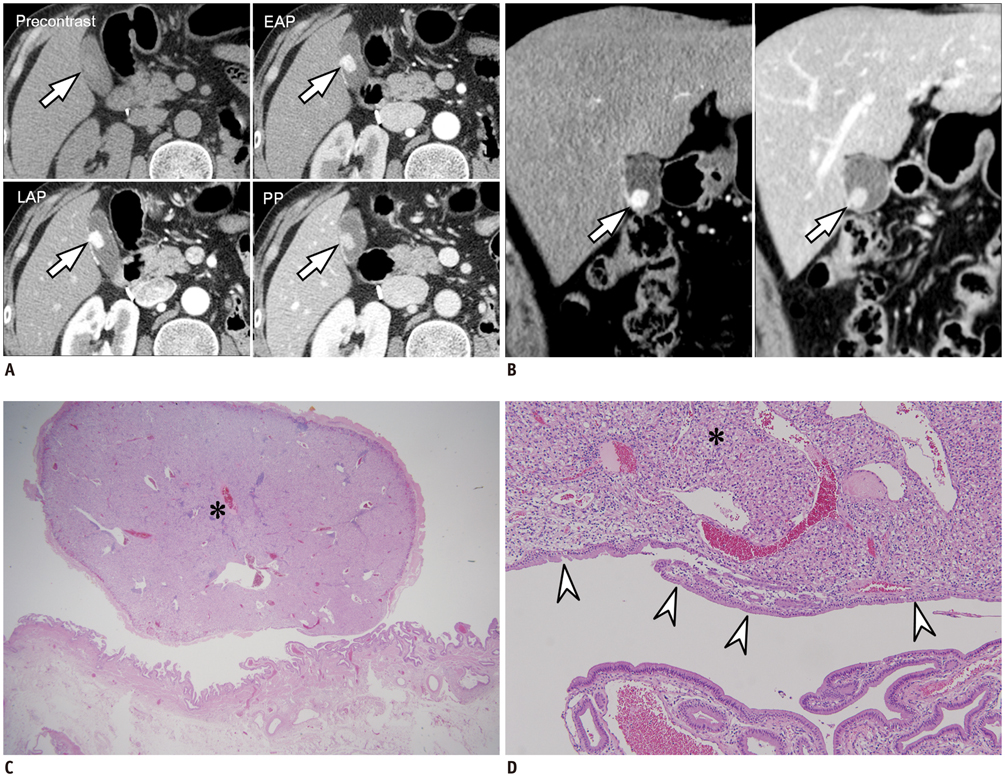
Twenty-one patients who had pathologically confirmed MGTs and underwent CT were retrospectively enrolled. Clinical findings including presenting symptoms, type of surgery, and interval between primary and metastatic tumors were recorded. Histologic features of primary tumor and MGTs including depth of invasion were also reviewed. Imaging findings were analyzed for the location and morphology of MGTs, pattern and degree of enhancement, depth of invasion, presence of intact overlying mucosa, and concordance between imaging features of primary and metastatic tumors. Significant differences between the histologies of MGTs and imaging features were determined.
RESULTS
The most common primary tumor metastasized to the GB was gastric cancer (n = 8), followed by renal cell carcinoma (n = 4) and hepatocellular carcinoma (n = 3). All MGTs (n = 21) manifested as infiltrative wall thickenings (n = 15) or as polypoid lesions (n = 6) on CT, similar to the features of primary GB cancers. There were significant differences in the morphology of MGTs, enhancement pattern, enhancement degree, and depth of invasion according to the histology of primary tumors (p < 0.05). Metastatic adenocarcinomas of the GB manifested as infiltrative and persistently enhancing wall thickenings, while non-adenocarcinomatous metastases usually manifested as polypoid lesions with early wash-in and wash-out.
CONCLUSION
Although CT findings of MGTs are similar to those of primary GB cancer, they are significantly different between the various histologies of primary tumors.
Keyword
MeSH Terms
-
Adenocarcinoma/pathology/radiography/secondary
Adult
Aged
Carcinoma, Hepatocellular/pathology/radiography/secondary
Carcinoma, Renal Cell/pathology/radiography/secondary
Carcinoma, Squamous Cell/pathology/radiography/secondary
Diagnosis, Differential
Female
Gallbladder Neoplasms/pathology/*radiography/*secondary
Humans
Kidney Neoplasms/pathology
Liver Neoplasms/pathology
Male
Melanoma/pathology/radiography/secondary
Middle Aged
Neoplasm Invasiveness/radiography
Retrospective Studies
Stomach Neoplasms/pathology
*Tomography, X-Ray Computed
Figure
Cited by 1 articles
-
Cavernous Hemangioma of the Gallbladder: a Case Report
Jae Hwi Park, Jeong Sub Lee, Guk Myung Choi, Bong Soo Kim, Seung Hyoung Kim, JeongJae Kim, Doo Ri Kim, Chang Lim Hyun, Kyu Hee Her
Investig Magn Reson Imaging. 2019;23(3):264-269. doi: 10.13104/imri.2019.23.3.264.
Reference
-
1. Yoon WJ, Yoon YB, Kim YJ, Ryu JK, Kim YT. Metastasis to the gallbladder: a single-center experience of 20 cases in South Korea. World J Gastroenterol. 2009; 15:4806–4809.2. Rehani B, Strohmeyer P, Jacobs M, Mantil J. Gallbladder metastasis from malignant melanoma: diagnosis with FDG PET/CT. Clin Nucl Med. 2006; 31:812–813.3. Guida M, Cramarossa A, Gentile A, Benvestito S, De Fazio M, Sanbiasi D, et al. Metastatic malignant melanoma of the gallbladder: a case report and review of the literature. Melanoma Res. 2002; 12:619–625.4. Vernadakis S, Rallis G, Danias N, Serafimidis C, Christodoulou E, Troullinakis M, et al. Metastatic melanoma of the gallbladder: an unusual clinical presentation of acute cholecystitis. World J Gastroenterol. 2009; 15:3434–3436.5. Ghaouti M, Znati K, Jahid A, Zouaidia F, Bernoussi Z, El Fakir Y, et al. A gallbladder tumor revealing metastatic clear cell renal carcinoma: report of case and review of literature. Diagn Pathol. 2013; 8:4.6. Chung PH, Srinivasan R, Linehan WM, Pinto PA, Bratslavsky G. Renal cell carcinoma with metastases to the gallbladder: four cases from the National Cancer Institute (NCI) and review of the literature. Urol Oncol. 2012; 30:476–481.7. Nojima H, Cho A, Yamamoto H, Nagata M, Takiguchi N, Kainuma O, et al. Renal cell carcinoma with unusual metastasis to the gallbladder. J Hepatobiliary Pancreat Surg. 2008; 15:209–212.8. Backman H. Metastases of malignant melanoma in the gastrointestinal tract. Geriatrics. 1969; 24:112–120.9. Barretta ML, Catalano O, Setola SV, Granata V, Marone U, D'Errico Gallipoli A. Gallbladder metastasis: spectrum of imaging findings. Abdom Imaging. 2011; 36:729–734.10. Kim SY, Kim KW, Kim AY, Ha HK, Kim JS, Park SH, et al. Bloodborne metastatic tumors to the gastrointestinal tract: CT findings with clinicopathologic correlation. AJR Am J Roentgenol. 2006; 186:1618–1626.11. Yoshimitsu K, Honda H, Shinozaki K, Aibe H, Kuroiwa T, Irie H, et al. Helical CT of the local spread of carcinoma of the gallbladder: evaluation according to the TNM system in patients who underwent surgical resection. AJR Am J Roentgenol. 2002; 179:423–428.12. Kim SJ, Lee JM, Lee JY, Choi JY, Kim SH, Han JK, et al. Accuracy of preoperative T-staging of gallbladder carcinoma using MDCT. AJR Am J Roentgenol. 2008; 190:74–80.13. Horton KM, Fishman EK. Current role of CT in imaging of the stomach. Radiographics. 2003; 23:75–87.14. Scatarige JC, DiSantis DJ. CT of the stomach and duodenum. Radiol Clin North Am. 1989; 27:687–706.15. Jin KN, Lee JM, Kim SH, Shin KS, Lee JY, Han JK, et al. The diagnostic value of multiplanar reconstruction on MDCT colonography for the preoperative staging of colorectal cancer. Eur Radiol. 2006; 16:2284–2291.16. Lee JH, Lee JM, Kim SJ, Baek JH, Yun SH, Kim KW, et al. Enhancement patterns of hepatocellular carcinomas on multiphasicmultidetector row CT: comparison with pathological differentiation. Br J Radiol. 2012; 85:e573–e583.17. Lee JM, Choi BI. Hepatocellular nodules in liver cirrhosis: MR evaluation. Abdom Imaging. 2011; 36:282–289.18. Sun MR, Ngo L, Genega EM, Atkins MB, Finn ME, Rofsky NM, et al. Renal cell carcinoma: dynamic contrast-enhanced MR imaging for differentiation of tumor subtypes--correlation with pathologic findings. Radiology. 2009; 250:793–802.19. Levy AD, Murakata LA, Rohrmann CA Jr. Gallbladder carcinoma: radiologic-pathologic correlation. Radiographics. 2001; 21:295–314. questionnaire, 549-555.20. Lane J, Buck JL, Zeman RK. Primary carcinoma of the gallbladder: a pictorial essay. Radiographics. 1989; 9:209–228.21. Ishiguro S, Onaya H, Esaki M, Kosuge T, Hiraoka N, Mizuguchi Y, et al. Mucin-producing carcinoma of the gallbladder: evaluation by magnetic resonance cholangiopancreatography in three cases. Korean J Radiol. 2012; 13:637–642.22. Westacott SM, Mahraj R. Anatomy and imaging of the normal gallbladder. In : Meilstrup JW, editor. Imaging atlas of the normal gallbladder and its variants. Boca Raton: CRC Press;1994. p. 4.23. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, et al. AJCC Cancer Staging Manual. 7th ed. New York: Springer-Verlag;2010. p. 211–217.24. Jang JY, Kim SW, Lee SE, Hwang DW, Kim EJ, Lee JY, et al. Differential diagnostic and staging accuracies of high resolution ultrasonography, endoscopic ultrasonography, and multidetector computed tomography for gallbladder polypoid lesions and gallbladder cancer. Ann Surg. 2009; 250:943–949.25. Jung SE, Lee JM, Lee K, Rha SE, Choi BG, Kim EK, et al. Gallbladder wall thickening: MR imaging and pathologic correlation with emphasis on layered pattern. Eur Radiol. 2005; 15:694–701.