Korean J Radiol.
2015 Apr;16(2):430-439. 10.3348/kjr.2015.16.2.430.
Digital Tomosynthesis for Evaluating Metastatic Lung Nodules: Nodule Visibility, Learning Curves, and Reading Times
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine, and Institute of Radiation Medicine, Seoul National University Medical Research Center, Seoul 110-744, Korea. jmgoo@plaza.snu.ac.kr
- 2Cancer Research Institute, Seoul National University College of Medicine, Seoul 110-744, Korea.
- KMID: 2070187
- DOI: http://doi.org/10.3348/kjr.2015.16.2.430
Abstract
OBJECTIVE
To evaluate nodule visibility, learning curves, and reading times for digital tomosynthesis (DT).
MATERIALS AND METHODS
We included 80 patients who underwent computed tomography (CT) and DT before pulmonary metastasectomy. One experienced chest radiologist annotated all visible nodules on thin-section CT scans using computer-aided detection software. Two radiologists used CT as the reference standard and retrospectively graded the visibility of nodules on DT. Nodule detection performance was evaluated in four sessions of 20 cases each by six readers. After each session, readers were unblinded to the DT images by revealing the true-positive markings and were instructed to self-analyze their own misreads. Receiver-operating-characteristic curves were determined.
RESULTS
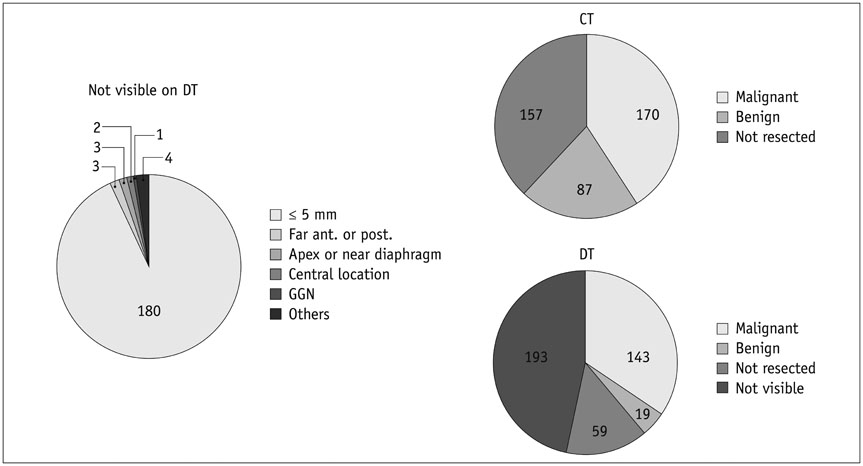
Among 414 nodules on CT, 53.3% (221/414) were visible on DT. The main reason for not seeing a nodule on DT was small size (93.3%, < or = 5 mm). DT revealed a substantial number of malignant nodules (84.1%, 143/170). The proportion of malignant nodules among visible nodules on DT was significantly higher (64.7%, 143/221) than that on CT (41.1%, 170/414) (p < 0.001). Area under the curve (AUC) values at the initial session were > 0.8, and the average detection rate for malignant nodules was 85% (210/246). The inter-session analysis of the AUC showed no significant differences among the readers, and the detection rate for malignant nodules did not differ across sessions. A slight improvement in reading times was observed.
CONCLUSION
Most malignant nodules > 5 mm were visible on DT. As nodule detection performance was high from the initial session, DT may be readily applicable for radiology residents and board-certified radiologists.
Keyword
MeSH Terms
Figure
Reference
-
1. Jung HN, Chung MJ, Koo JH, Kim HC, Lee KS. Digital tomosynthesis of the chest: utility for detection of lung metastasis in patients with colorectal cancer. Clin Radiol. 2012; 67:232–238.2. Dobbins JT 3rd, McAdams HP. Chest tomosynthesis: technical principles and clinical update. Eur J Radiol. 2009; 72:244–251.3. Yamada Y, Jinzaki M, Hasegawa I, Shiomi E, Sugiura H, Abe T, et al. Fast scanning tomosynthesis for the detection of pulmonary nodules: diagnostic performance compared with chest radiography, using multidetector-row computed tomography as the reference. Invest Radiol. 2011; 46:471–477.4. James TD, McAdams HP, Song JW, Li CM, Godfrey DJ, DeLong DM, et al. Digital tomosynthesis of the chest for lung nodule detection: interim sensitivity results from an ongoing NIH-sponsored trial. Med Phys. 2008; 35:2554–2557.5. Vikgren J, Zachrisson S, Svalkvist A, Johnsson AA, Boijsen M, Flinck A, et al. Comparison of chest tomosynthesis and chest radiography for detection of pulmonary nodules: human observer study of clinical cases. Radiology. 2008; 249:1034–1041.6. Potchen EJ, Cooper TG, Sierra AE, Aben GR, Potchen MJ, Potter MG, et al. Measuring performance in chest radiography. Radiology. 2000; 217:456–459.7. Asplund S, Johnsson AA, Vikgren J, Svalkvist A, Boijsen M, Fisichella V, et al. Learning aspects and potential pitfalls regarding detection of pulmonary nodules in chest tomosynthesis and proposed related quality criteria. Acta Radiol. 2011; 52:503–512.8. Dachman AH, Kelly KB, Zintsmaster MP, Rana R, Khankari S, Novak JD, et al. Formative evaluation of standardized training for CT colonographic image interpretation by novice readers. Radiology. 2008; 249:167–177.9. Hock D, Ouhadi R, Materne R, Aouchria AS, Mancini I, Broussaud T, et al. Virtual dissection CT colonography: evaluation of learning curves and reading times with and without computer-aided detection. Radiology. 2008; 248:860–868.10. Otani H, Nitta N, Ikeda M, Nagatani Y, Tanaka T, Kitahara H, et al. Flat-panel detector computed tomography imaging: observer performance in detecting pulmonary nodules in comparison with conventional chest radiography and multidetector computed tomography. J Thorac Imaging. 2012; 27:51–57.11. Monnier-Cholley L, Carrat F, Cholley BP, Tubiana JM, Arrivé L. Detection of lung cancer on radiographs: receiver operating characteristic analyses of radiologists', pulmonologists', and anesthesiologists' performance. Radiology. 2004; 233:799–805.12. Kakeda S, Moriya J, Sato H, Aoki T, Watanabe H, Nakata H, et al. Improved detection of lung nodules on chest radiographs using a commercial computer-aided diagnosis system. AJR Am J Roentgenol. 2004; 182:505–510.13. Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983; 148:839–843.14. Fischbach F, Knollmann F, Griesshaber V, Freund T, Akkol E, Felix R. Detection of pulmonary nodules by multislice computed tomography: improved detection rate with reduced slice thickness. Eur Radiol. 2003; 13:2378–2383.15. Goo JM. A computer-aided diagnosis for evaluating lung nodules on chest CT: the current status and perspective. Korean J Radiol. 2011; 12:145–155.16. Park EA, Goo JM, Lee JW, Kang CH, Lee HJ, Lee CH, et al. Efficacy of computer-aided detection system and thin-slab maximum intensity projection technique in the detection of pulmonary nodules in patients with resected metastases. Invest Radiol. 2009; 44:105–113.17. Quaia E, Baratella E, Cioffi V, Bregant P, Cernic S, Cuttin R, et al. The value of digital tomosynthesis in the diagnosis of suspected pulmonary lesions on chest radiography: analysis of diagnostic accuracy and confidence. Acad Radiol. 2010; 17:1267–1274.18. Quaia E, Baratella E, Poillucci G, Kus S, Cioffi V, Cova MA. Digital tomosynthesis as a problem-solving imaging technique to confirm or exclude potential thoracic lesions based on chest X-ray radiography. Acad Radiol. 2013; 20:546–553.19. Kim EY, Chung MJ, Choe YH, Lee KS. Digital tomosynthesis for aortic arch calcification evaluation: performance comparison with chest radiography with CT as the reference standard. Acta Radiol. 2012; 53:17–22.20. Rose SL, Tidwell AL, Bujnoch LJ, Kushwaha AC, Nordmann AS, Sexton R Jr. Implementation of breast tomosynthesis in a routine screening practice: an observational study. AJR Am J Roentgenol. 2013; 200:1401–1408.21. Lee G, Jeong YJ, Kim KI, Song JW, Kang DM, Kim YD, et al. Comparison of chest digital tomosynthesis and chest radiography for detection of asbestos-related pleuropulmonary disease. Clin Radiol. 2013; 68:376–382.22. Quaia E, Baratella E, Cernic S, Lorusso A, Casagrande F, Cioffi V, et al. Analysis of the impact of digital tomosynthesis on the radiological investigation of patients with suspected pulmonary lesions on chest radiography. Eur Radiol. 2012; 22:1912–1922.23. Terzi A, Bertolaccini L, Viti A, Comello L, Ghirardo D, Priotto R, et al. Lung cancer detection with digital chest tomosynthesis: baseline results from the observational study SOS. J Thorac Oncol. 2013; 8:685–692.24. Kim EY, Chung MJ, Lee HY, Koh WJ, Jung HN, Lee KS. Pulmonary mycobacterial disease: diagnostic performance of low-dose digital tomosynthesis as compared with chest radiography. Radiology. 2010; 257:269–277.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Application of Artificial Intelligence in Digital Breast Tomosynthesis
- Digital Tomosynthesis of the Chest: Comparison of Patient Exposure Dose and Image Quality between Standard Default Setting and Low Dose Setting
- A Computer-Aided Diagnosis for Evaluating Lung Nodules on Chest CT: the Current Status and Perspective
- Digital Tomosynthesis for Patient Alignment System Using Half-fan Mode CBCT Projection Images
- Fate of pulmonary nodules detected by computer-aided diagnosis and physician review on the computed tomography simulation images for hepatocellular carcinoma