Yonsei Med J.
2015 Mar;56(2):375-381. 10.3349/ymj.2015.56.2.375.
The Characteristics of Recurrent Upper Tract Urothelial Carcinoma after Radical Nephroureterectomy without Bladder Cuff Excision
- Affiliations
-
- 1Department of Urology, Seoul National University Hospital, Seoul, Korea. kuuro70@snu.ac.kr
- KMID: 2070013
- DOI: http://doi.org/10.3349/ymj.2015.56.2.375
Abstract
- PURPOSE
To investigate oncological outcomes based on bladder cuff excision (BCE) during radical nephroureterectomy (RNU) for upper tract urothelial carcinoma (UTUC) and to provide clinical evidence of tumor recurrence in patients without BCE.
MATERIALS AND METHODS
We retrospectively collected data of 372 consecutive patients who underwent RNU at our institution from May 1989 through October 2010. After excluding some data, we reviewed 336 patients for the analysis.
RESULTS
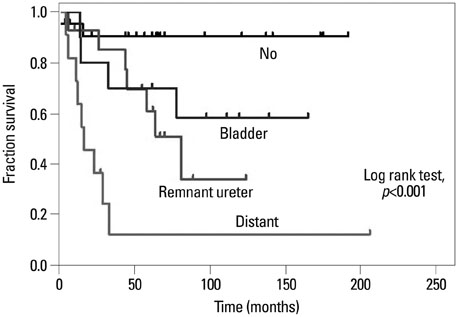
Of the patients who underwent RNU with BCE (n=279, 83.0%) and without BCE (n=57, 17.0%), patients without BCE had poorer cancer-specific and overall survival rates. Among 57 patients without BCE, 35 (61.4%) experienced tumor recurrence. Recurrence at the remnant ureter resulted in poor oncological outcomes compared to those in patients with bladder recurrence, but better outcomes were observed compared to recurrence at other sites. No significant predictors for tumor recurrence at the remnant ureter were identified. In patients without BCE, pathological T stage [hazard ratio (HR), 5.73] and lymphovascular invasion (HR, 3.65) were independent predictors of cancer-specific survival, whereas age (HR, 1.04), pathological T stage (HR, 5.11), and positive tumor margin (HR, 6.50) were independent predictors of overall survival.
CONCLUSION
Patients without BCE had poorer overall and cancer-specific survival after RNU than those with BCE. Most of these patients experienced tumor recurrence at the remnant ureter and other sites. Patients with non-organ confined UTUC after RNU without BCE may be considered for adjuvant chemotherapy with careful follow-up.
Keyword
MeSH Terms
-
Adult
Aged
Carcinoma, Transitional Cell/*surgery
Chemotherapy, Adjuvant
Female
Humans
Male
Middle Aged
Neoplasm Recurrence, Local/*pathology
Nephrectomy/*methods
Retrospective Studies
Survival Rate
Treatment Outcome
Ureter/*surgery
Ureteral Neoplasms/*surgery
Urinary Bladder/pathology
Urinary Bladder Neoplasms/*pathology
Urologic Neoplasms/pathology/*surgery
*Urologic Surgical Procedures
Urothelium/*pathology
Figure
Reference
-
1. Kirkali Z, Tuzel E. Transitional cell carcinoma of the ureter and renal pelvis. Crit Rev Oncol Hematol. 2003; 47:155–169.
Article2. Kirkali Z, Chan T, Manoharan M, Algaba F, Busch C, Cheng L, et al. Bladder cancer: epidemiology, staging and grading, and diagnosis. Urology. 2005; 66:6 Suppl 1. 4–34.
Article3. Munoz JJ, Ellison LM. Upper tract urothelial neoplasms: incidence and survival during the last 2 decades. J Urol. 2000; 164:1523–1525.
Article4. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013; 63:11–30.
Article5. Booth CM, Cameron KM, Pugh RC. Urothelial carcinoma of the kidney and ureter. Br J Urol. 1980; 52:430–435.
Article6. McCarron JP, Mills C, Vaughn ED Jr. Tumors of the renal pelvis and ureter: current concepts and management. Semin Urol. 1983; 1:75–81.7. Rouprêt M, Babjuk M, Compérat E, Zigeuner R, Sylvester R, Burger M, et al. European guidelines on upper tract urothelial carcinomas: 2013 update. Eur Urol. 2013; 63:1059–1071.
Article8. Srirangam SJ, van Cleynenbreugel B, van Poppel H. Laparoscopic nephroureterectomy: the distal ureteral dilemma. Adv Urol. 2009; 316807.
Article9. Zlotta AR. Should urologists always perform a bladder cuff resection during nephroureterectomy, and which method should they use? Eur Urol. 2010; 57:970–972.
Article10. Lughezzani G, Sun M, Perrotte P, Shariat SF, Jeldres C, Budaus L, et al. Should bladder cuff excision remain the standard of care at nephroureterectomy in patients with urothelial carcinoma of the renal pelvis? A population-based study. Eur Urol. 2010; 57:956–962.
Article11. Lughezzani G, Jeldres C, Isbarn H, Sun M, Shariat SF, Alasker A, et al. Nephroureterectomy and segmental ureterectomy in the treatment of invasive upper tract urothelial carcinoma: a population-based study of 2299 patients. Eur J Cancer. 2009; 45:3291–3297.
Article12. Hou CP, Chang PL, Chen CL, Lin YH, Tsui KH. Does adequate bladder cuff excision impact outcomes in patients undergoing nephroureterectomy for upper tract urothelial carcinoma. Chang Gung Med J. 2011; 34:496–505.13. Cha EK, Shariat SF, Kormaksson M, Novara G, Chromecki TF, Scherr DS, et al. Predicting clinical outcomes after radical nephroureterectomy for upper tract urothelial carcinoma. Eur Urol. 2012; 61:818–825.
Article14. Jeldres C, Lughezzani G, Sun M, Isbarn H, Shariat SF, Budaus L, et al. Segmental ureterectomy can safely be performed in patients with transitional cell carcinoma of the ureter. J Urol. 2010; 183:1324–1329.
Article15. Fairey AS, Kassouf W, Estey E, Tanguay S, Rendon R, Bell D, et al. Comparison of oncological outcomes for open and laparoscopic radical nephroureterectomy: results from the Canadian Upper Tract Collaboration. BJU Int. 2013; 112:791–797.
Article16. Hung SY, Yang WC, Luo HL, Hsu CC, Chen YT, Chuang YC. Segmental ureterectomy does not compromise the oncologic outcome compared with nephroureterectomy for pure ureter cancer. Int Urol Nephrol. 2014; 46:921–926.
Article17. Ko R, Chew BH, Hickling DR, Razvi H, Luke PP, Chin JL, et al. Transitional-cell carcinoma recurrence rate after nephroureterectomy in patients who undergo open excision of bladder cuff v transurethral incision of the ureteral orifice. J Endourol. 2007; 21:730–734.
Article18. Abel EJ, Fisher MB, Matin SF, Kamat AM, Dinney CP, Grossman HB. Delayed ureterectomy after incomplete nephroureterectomy for upper tract urothelial carcinoma: pathologic findings and outcomes. Int Braz J Urol. 2013; 39:817–822.
Article19. Huben RP, Mounzer AM, Murphy GP. Tumor grade and stage as prognostic variables in upper tract urothelial tumors. Cancer. 1988; 62:2016–2020.
Article20. Oosterlinck W, Solsona E, van der Meijden AP, Sylvester R, Böhle A, Rintala E, et al. EAU guidelines on diagnosis and treatment of upper urinary tract transitional cell carcinoma. Eur Urol. 2004; 46:147–154.
Article21. Oikawa T, Nomura H, Kinsui H, Hamano S, Suzuki N, Tanaka M, et al. [A clinicopathological evaluation of prognostic factors of urothelial tumors of the renal pelvis and ureter]. Hinyokika Kiyo. 2001; 47:237–240.22. Colin P, Ouzzane A, Pignot G, Ravier E, Crouzet S, Ariane MM, et al. Comparison of oncological outcomes after segmental ureterectomy or radical nephroureterectomy in urothelial carcinomas of the upper urinary tract: results from a large French multicentre study. BJU Int. 2012; 110:1134–1141.
Article23. Espiritu PN, Sverrisson EF, Sexton WJ, Pow-Sang JM, Poch MA, Dhillon J, et al. Effect of tumor size on recurrence-free survival of upper tract urothelial carcinoma following surgical resection. Urol Oncol. 2014; 32:619–624.
Article24. Margulis V, Youssef RF, Karakiewicz PI, Lotan Y, Wood CG, Zigeuner R, et al. Preoperative multivariable prognostic model for prediction of nonorgan confined urothelial carcinoma of the upper urinary tract. J Urol. 2010; 184:453–458.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Urothelial Tumors of the Upper Urinary Tract: Multiplicity and Prognostic Variables
- Transitional Cell Carcinoma of Renal Pelvis Treated by Nephroureterectomy with Endoscopic Bladder Cuff Resection
- Effects of Complete Bladder Cuff Removal on Oncological Outcomes Following Radical Nephroureterectomy for Upper Tract Urothelial Carcinoma
- Urothelial Tumors of the Upper Urinary Tract, 15 Cases
- Pathologic Features of Recurrent Bladder Tumors after Upper Urinary Tract Transitional Cell Carcinoma