Clin Orthop Surg.
2015 Mar;7(1):91-96. 10.4055/cios.2015.7.1.91.
Perioperative Surgical Complications and Learning Curve Associated with Minimally Invasive Transforaminal Lumbar Interbody Fusion: A Single-Institute Experience
- Affiliations
-
- 1Department of Orthopedic Surgery, National Health Insurance Service Ilsan Hospital, Yonsei University College of Medicine, Goyang, Korea. yungspine@gmail.com
- KMID: 2069880
- DOI: http://doi.org/10.4055/cios.2015.7.1.91
Abstract
- BACKGROUND
As surgical complications tend to occur more frequently in the beginning stages of a surgeon's career, knowledge of perioperative complications is important to perform a safe procedure, especially if the surgeon is a novice. We sought to identify and describe perioperative complications and their management in connection with minimally invasive transforaminal lumbar interbody fusion (TLIF).
METHODS
We performed a retrospective chart review of our first 124 patients who underwent minimally invasive TLIF. The primary outcome measure was adverse events during the perioperative period, including neurovascular injury, implant-related complications, and wound infection. Pseudarthroses and adjacent segment pathologies were not included in this review. Adverse events that were not specifically related to spinal surgery and did not affect recovery were also excluded.
RESULTS
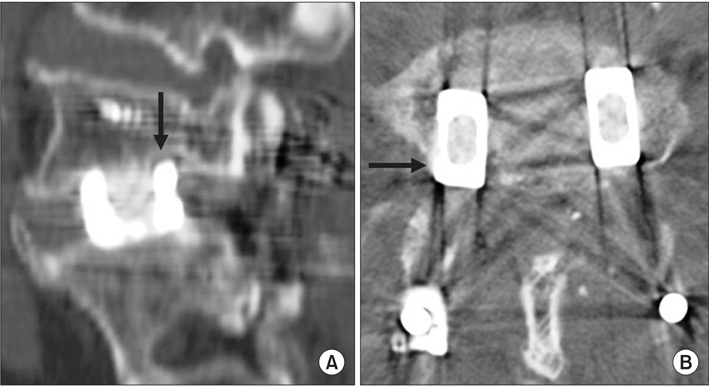
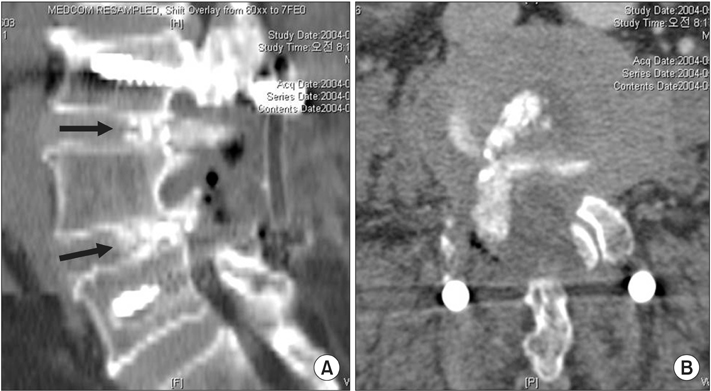
Perioperative complications occurred in 9% of patients (11/124); including three cases of temporary postoperative neuralgia, two deep wound infections, two pedicle screw misplacements, two cage migrations, one dural tear, and one grafted bone extrusion. No neurologic deficits were reported. Eight complications occurred in the first one-third of the series and only 3 complications occurred in the last two-thirds of the series. Additional surgeries were performed in 6% of patients (7/124); including four reoperations (two for cage migrations, one for a misplaced screw, and one for an extruded graft bone fragment) and three hardware removals (one for a misplaced screw and two for infected cages).
CONCLUSIONS
We found perioperative complications occurred more often in the early period of a surgeon's experience with minimally invasive TLIF. Implant-related complications were common and successfully managed by additional surgeries in this series. We suggest greater caution should be exercised to avoid the potential complications, especially when surgeon is a novice to this procedure.
MeSH Terms
Figure
Cited by 1 articles
-
Surgical Strategies for Successful Minimally Invasive Transforaminal Lumbar Interbody Fusion
Yung Park, Se-Jun Park, Jae-Young Hong, Ki-Hyoung Koo
J Korean Soc Spine Surg. 2016;23(4):251-261. doi: 10.4184/jkss.2016.23.4.251.
Reference
-
1. Dhall SS, Wang MY, Mummaneni PV. Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up. J Neurosurg Spine. 2008; 9(6):560–565.
Article2. Peng CW, Yue WM, Poh SY, Yeo W, Tan SB. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine (Phila Pa 1976). 2009; 34(13):1385–1389.
Article3. Scheufler KM, Dohmen H, Vougioukas VI. Percutaneous transforaminal lumbar interbody fusion for the treatment of degenerative lumbar instability. Neurosurgery. 2007; 60:4 Suppl 2. 203–212.
Article4. Schizas C, Tzinieris N, Tsiridis E, Kosmopoulos V. Minimally invasive versus open transforaminal lumbar interbody fusion: evaluating initial experience. Int Orthop. 2009; 33(6):1683–1688.
Article5. Shunwu F, Xing Z, Fengdong Z, Xiangqian F. Minimally invasive transforaminal lumbar interbody fusion for the treatment of degenerative lumbar diseases. Spine (Phila Pa 1976). 2010; 35(17):1615–1620.
Article6. Lau D, Lee JG, Han SJ, Lu DC, Chou D. Complications and perioperative factors associated with learning the technique of minimally invasive transforaminal lumbar interbody fusion (TLIF). J Clin Neurosci. 2011; 18(5):624–627.
Article7. Lee JC, Jang HD, Shin BJ. Learning curve and clinical outcomes of minimally invasive transforaminal lumbar interbody fusion: our experience in 86 consecutive cases. Spine (Phila Pa 1976). 2012; 37(18):1548–1557.
Article8. Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Minimally invasive or open transforaminal lumbar interbody fusion as revision surgery for patients previously treated by open discectomy and decompression of the lumbar spine. Eur Spine J. 2011; 20(4):623–628.
Article9. Schizas C, Michel J, Kosmopoulos V, Theumann N. Computer tomography assessment of pedicle screw insertion in percutaneous posterior transpedicular stabilization. Eur Spine J. 2007; 16(5):613–617.
Article10. Aoki Y, Yamagata M, Nakajima F, et al. Examining risk factors for posterior migration of fusion cages following transforaminal lumbar interbody fusion: a possible limitation of unilateral pedicle screw fixation. J Neurosurg Spine. 2010; 13(3):381–387.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Complications of Minimally Invasive Transforaminal Lumbar Interbody Fusion
- Minimally Invasive Strategy for Uniportal Full-Endoscopic Transforaminal Lumbar Interbody Fusion Using a Large Cage Utilized in Oblique Lumbar Interbody Fusion
- Biportal Endoscopic Transforaminal Lumbar Interbody Fusion with Percutaneous Instrumentation: A Technical Note
- Minimally Invasive Lateral Lumbar Interbody Fusion: Indications, Outcomes and Complications
- Biportal Endoscopic Transforaminal Interbody Fusion for Lumbar Adjacent Segment Disease: An Illustrative Case and Literature Review