J Korean Neurosurg Soc.
2015 Jul;58(1):43-49. 10.3340/jkns.2015.58.1.43.
The Change of Sagittal Alignment of the Lumbar Spine after Dynesys Stabilization and Proposal of a Refinement
- Affiliations
-
- 1Department of Mechanical Engineering, Kyung Hee University, Yongin, Korea.
- 2Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea. chungc@snu.ac.kr
- 3Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea.
- 4Neuroscience Research Institute, Seoul National University Medical Research Center, Seoul, Korea.
- 5Clinical Research Institute, Seoul National University Hospital, Seoul, Korea.
- 6Department of Brain and Cognitive Sciences, Seoul National University College of Natural Sciences, Seoul, Korea.
- 7Department of Neurosurgery, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2067103
- DOI: http://doi.org/10.3340/jkns.2015.58.1.43
Abstract
OBJECTIVE
Dynesys(R) is one of the pedicle-based dynamic lumbar stabilization systems and good clinical outcome has been reported. However, the cylindrical spacer between the heads of the screws undergoes deformation during assembly of the system. The pre-strain probably change the angle of instrumented spine with time and oblique-shaped spacer may reduce the pre-strain. We analyzed patients with single-level stabilization with Dynesys(R) and simulated oblique-shaped spacer with finite element (FE) model analysis.
METHODS
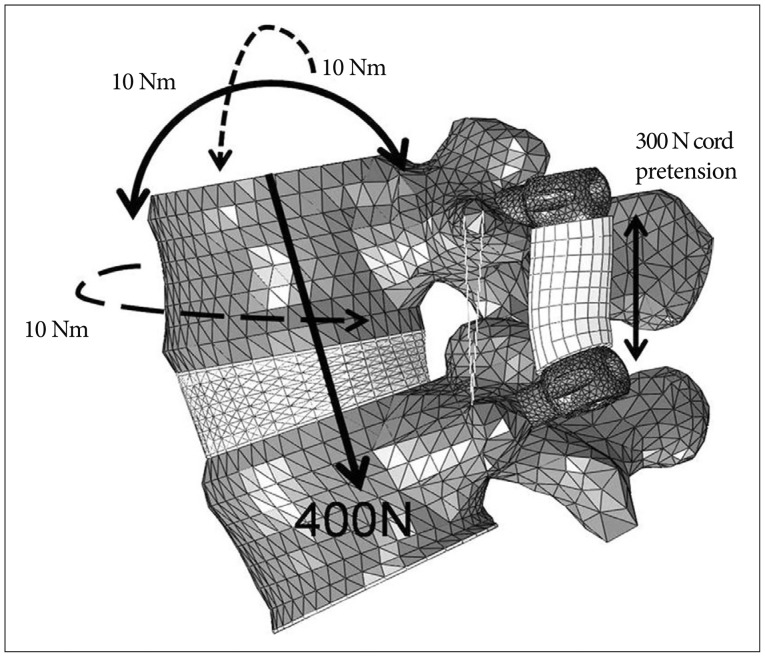
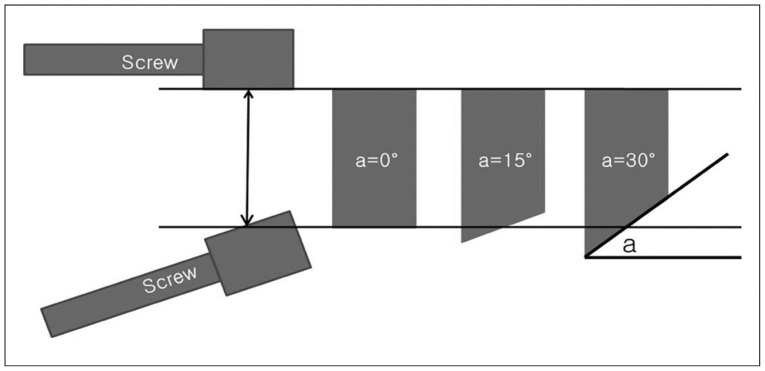
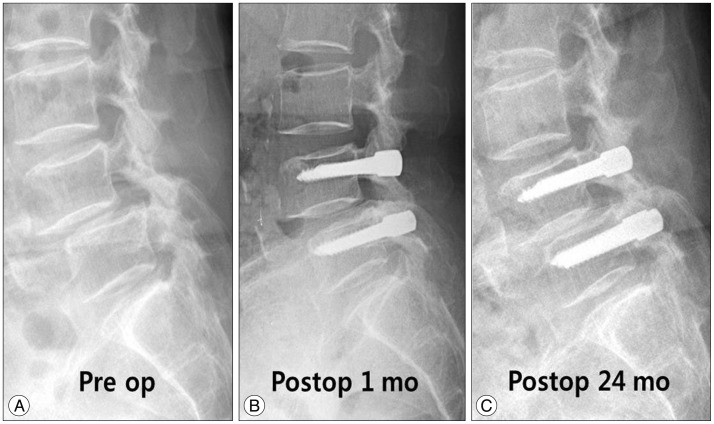
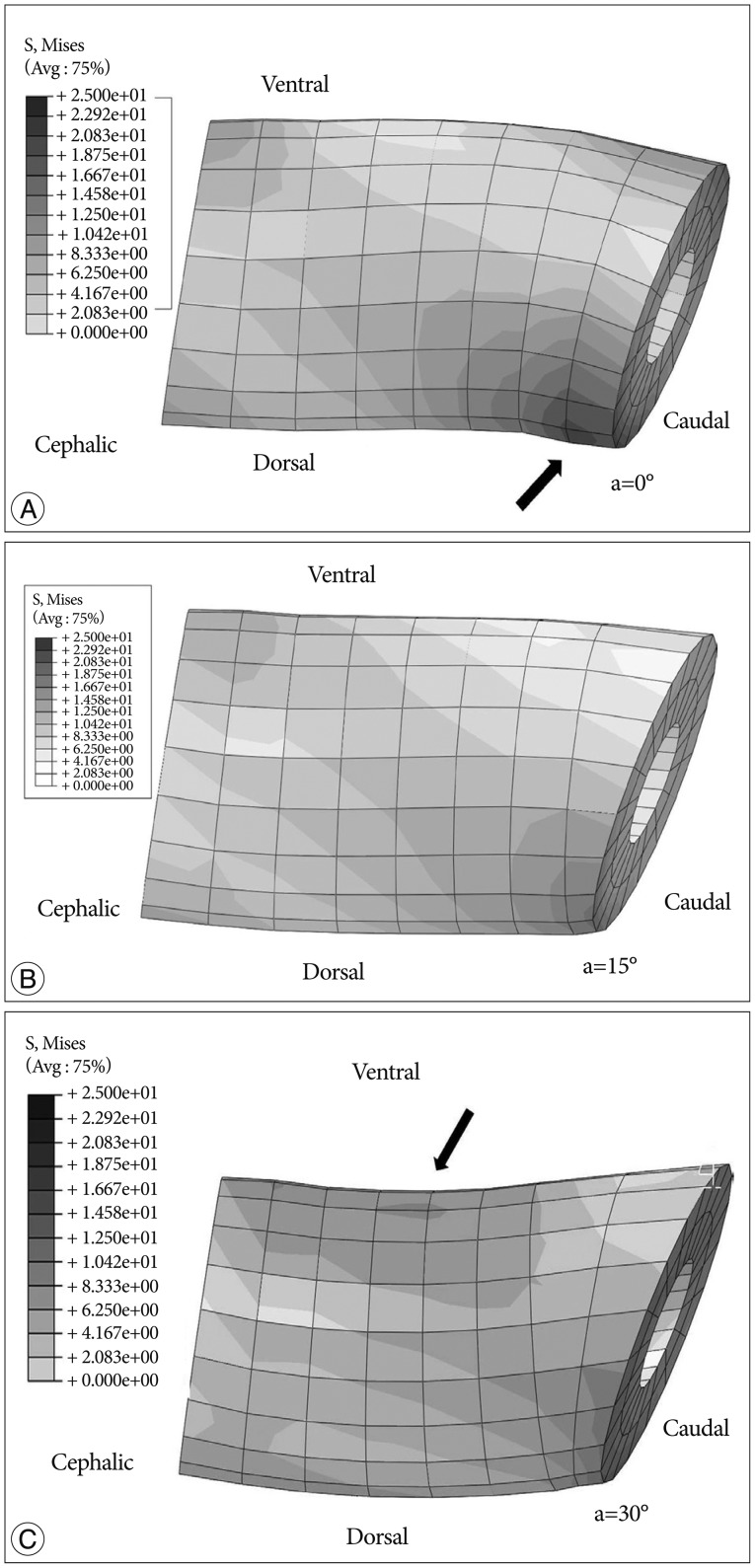
Consecutive 14 patients, who underwent surgery for single-level lumbar spinal stenosis and were followed-up more than 24 months (M : F=6 : 8; age, 58.7+/-8.0 years), were analyzed. Lumbar lordosis and segmental angle at the index level were compared between preoperation and postoperative month 24. The von Mises stresses on the obliquely-cut spacer (5degrees, 10degrees, 15degrees, 20degrees, 25degrees, and 30degrees) were calculated under the compressive force of 400 N and 10 Nm of moment with validated FE model of the L4-5 spinal motion segment with segmental angle of 16degrees.
RESULTS
Lumbar lordosis was not changed, while segmental angle was changed significantly from -8.1+/-7.2degrees to -5.9+/-6.7degrees (p<0.01) at postoperative month 24. The maximum von Mises stresses were markedly decreased with increased angle of the spacer up to 20degrees. The stress on the spacer was uneven with cylindrical spacer but it became even with the 15degrees oblique spacer.
CONCLUSION
The decreased segmental lordosis may be partially related to the pre-strain of Dynesys. Further clinical and biomechanical studies are required for relevant use of the system.
Figure
Reference
-
1. Barrey C, Jund J, Noseda O, Roussouly P. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J. 2007; 16:1459–1467. PMID: 17211522.
Article2. Bellini CM, Galbusera F, Raimondi MT, Mineo GV, Brayda-Bruno M. Biomechanics of the lumbar spine after dynamic stabilization. J Spinal Disord Tech. 2007; 20:423–429. PMID: 17970182.
Article3. Bothmann M, Kast E, Boldt GJ, Oberle J. Dynesys fixation for lumbar spine degeneration. Neurosurg Rev. 2008; 31:189–196. PMID: 17906883.
Article4. Chien CY, Tan CH, Lu TH, Lin SC, Chuang WH, Chiang MC, et al. Pretension effects of the Dynesys cord on the tissue responses and screw-spacer behaviors of the lumbosacral construct with hybrid fixation. Spine (Phila Pa 1976). 2013; 38:E775–E782. PMID: 23486410.
Article5. Cunningham BW, Dawson JM, Hu N, Kim SW, McAfee PC, Griffith SL. Preclinical evaluation of the Dynesys posterior spinal stabilization system : a nonhuman primate model. Spine J. 2010; 10:775–783. PMID: 20494624.
Article6. Dakhil-Jerew F, Jadeja H, Cohen A, Shepperd JA. Inter-observer reliability of detecting Dynesys pedicle screw using plain X-rays : a study on 50 post-operative patients. Eur Spine J. 2009; 18:1486–1493. PMID: 19533178.
Article7. Fay LY, Wu JC, Tsai TY, Wu CL, Huang WC, Cheng H. Dynamic stabilization for degenerative spondylolisthesis : evaluation of radiographic and clinical outcomes. Clin Neurol Neurosurg. 2013; 115:535–541. PMID: 22727211.
Article8. Gédet P, Haschtmann D, Thistlethwaite PA, Ferguson SJ. Comparative biomechanical investigation of a modular dynamic lumbar stabilization system and the Dynesys system. Eur Spine J. 2009; 18:1504–1511. PMID: 19565278.
Article9. Grob D, Benini A, Junge A, Mannion AF. Clinical experience with the Dynesys semirigid fixation system for the lumbar spine : surgical and patient-oriented outcome in 50 cases after an average of 2 years. Spine (Phila Pa 1976). 2005; 30:324–331. PMID: 15682014.
Article10. Hammerberg EM, Wood KB. Sagittal profile of the elderly. J Spinal Disord Tech. 2003; 16:44–50. PMID: 12571484.
Article11. Ianuzzi A, Kurtz SM, Kane W, Shah P, Siskey R, van Ooij A, et al. In vivo deformation, surface damage, and biostability of retrieved Dynesys systems. Spine (Phila Pa 1976). 2010; 35:E1310–E1316. PMID: 20975485.
Article12. Iguchi T, Ozaki T, Chin T, Tsumura N, Kanemura A, Kasahara K, et al. Intimate relationship between instability and degenerative signs at L4/5 segment examined by flexion-extension radiography. Eur Spine J. 2011; 20:1349–1354. PMID: 21509654.
Article13. Kim CH, Chung CK, Hong HS, Kim EH, Kim MJ, Park BJ. Validation of a simple computerized tool for measuring spinal and pelvic parameters. J Neurosurg Spine. 2012; 16:154–162. PMID: 22136391.
Article14. Kim CH, Chung CK, Jahng TA. Comparisons of outcomes after single or multilevel dynamic stabilization : effects on adjacent segment. J Spinal Disord Tech. 2011; 24:60–67. PMID: 21270627.
Article15. Kim DY, Lee SH, Lee HY, Lee HJ, Chang SB, Chung SK, et al. Validation of the Korean version of the oswestry disability index. Spine (Phila Pa 1976). 2005; 30:E123–E127. PMID: 15738775.
Article16. Kim KT, Lee SH, Suk KS, Lee JH, Jeong BO. Biomechanical changes of the lumbar segment after total disc replacement : chariter, prodiscr and maverickr using finite element model study. J Korean Neurosurg Soc. 2010; 47:446–453. PMID: 20617091.
Article17. Kim SM, Yang IC, Lee SY, Cho SY. Dynamic simulation of universal spacer in Dynesys dynamic stabilization system for human vertebra. T Nonferr Metal Soc. 2009; 19:S238–S242.
Article18. Ko CC, Tsai HW, Huang WC, Wu JC, Chen YC, Shih YH, et al. Screw loosening in the Dynesys stabilization system : radiographic evidence and effect on outcomes. Neurosurg Focus. 2010; 28:E10. PMID: 20568916.19. Kocak T, Cakir B, Reichel H, Mattes T. Screw loosening after posterior dynamic stabilization--review of the literature. Acta Chir Orthop Traumatol Cech. 2010; 77:134–139. PMID: 20447357.20. Liu CL, Zhong ZC, Hsu HW, Shih SL, Wang ST, Hung C, et al. Effect of the cord pretension of the Dynesys dynamic stabilisation system on the biomechanics of the lumbar spine : a finite element analysis. Eur Spine J. 2011; 20:1850–1858. PMID: 21523456.
Article21. Liu CL, Zhong ZC, Shih SL, Hung C, Lee YE, Chen CS. Influence of Dynesys system screw profile on adjacent segment and screw. J Spinal Disord Tech. 2010; 23:410–417. PMID: 20683426.
Article22. Markwalder TM, Wenger M. Dynamic stabilization of lumbar motion segments by use of Graf’s ligaments : results with an average follow-up of 7.4 years in 39 highly selected, consecutive patients. Acta Neurochir (Wien). 2003; 145:209–214. discussion 214. PMID: 12632117.
Article23. Meyers K, Tauber M, Sudin Y, Fleischer S, Arnin U, Girardi F, et al. Use of instrumented pedicle screws to evaluate load sharing in posterior dynamic stabilization systems. Spine J. 2008; 8:926–932. PMID: 18037350.
Article24. Mulholland RC, Sengupta DK. Rationale, principles and experimental evaluation of the concept of soft stabilization. Eur Spine J. 2002; (11 Suppl 2):S198–S205. PMID: 12384745.
Article25. Nockels RP. Dynamic stabilization in the surgical management of painful lumbar spinal disorders. Spine (Phila Pa 1976). 2005; 30(16 Suppl):S68–S72. PMID: 16103836.
Article26. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion : review of the literature. Spine (Phila Pa 1976). 2004; 29:1938–1944. PMID: 15534420.
Article27. Park WM, Kim K, Kim YH. Effects of degenerated intervertebral discs on intersegmental rotations, intradiscal pressures, and facet joint forces of the whole lumbar spine. Comput Biol Med. 2013; 43:1234–1240. PMID: 23930818.
Article28. Sapkas GS, Themistocleous GS, Mavrogenis AF, Benetos IS, Metaxas N, Papagelopoulos PJ. Stabilization of the lumbar spine using the dynamic neutralization system. Orthopedics. 2007; 30:859–865. PMID: 17990413.
Article29. Schaeren S, Broger I, Jeanneret B. Minimum four-year follow-up of spinal stenosis with degenerative spondylolisthesis treated with decompression and dynamic stabilization. Spine (Phila Pa 1976). 2008; 33:E636–E642. PMID: 18708915.
Article30. Schnake KJ, Schaeren S, Jeanneret B. Dynamic stabilization in addition to decompression for lumbar spinal stenosis with degenerative spondylolisthesis. Spine (Phila Pa 1976). 2006; 31:442–429. PMID: 16481955.
Article31. Schulte TL, Hurschler C, Haversath M, Liljenqvist U, Bullmann V, Filler TJ, et al. The effect of dynamic, semi-rigid implants on the range of motion of lumbar motion segments after decompression. Eur Spine J. 2008; 17:1057–1065. PMID: 18493802.
Article32. Schwarzenbach O, Berlemann U, Stoll TM, Dubois G. Posterior dynamic stabilization systems : Dynesys. Orthop Clin North Am. 2005; 36:363–372. PMID: 15950696.33. Sengupta DK. Dynamic stabilization devices in the treatment of low back pain. Neurol India. 2005; 53:466–474. PMID: 16565539.
Article34. Stoll TM, Dubois G, Schwarzenbach O. The dynamic neutralization system for the spine : a multi-center study of a novel non-fusion system. Eur Spine J. 11(Suppl 2):2002; S170–S178. PMID: 12384741.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Screw loosening and Migration after Dynesys Implantation
- Analysis of the Sagittal Alignment of Normal Spines
- The Role of the Pelvis in Sagittal Alignment of Lumbar Degenerative Disease Patients
- Cervical Sagittal Alignment: Literature Review and Future Directions
- From the Spinopelvic Parameters to Global Alignment and Proportion Scores in Adult Spinal Deformity