Korean J Urol.
2013 May;54(5):327-332. 10.4111/kju.2013.54.5.327.
Laparoendoscopic Single-Site Surgery With the Second-Generation Single Port Instrument Delivery Extended Reach Surgical System in a Porcine Model
- Affiliations
-
- 1Department of Urology, Dong-A Medical Center, Busan, Korea. sunggt@daunet.donga.ac.kr
- 2Department of Urology, University of California Irvine Medical Center, Irvine, CA, USA.
- KMID: 2061515
- DOI: http://doi.org/10.4111/kju.2013.54.5.327
Abstract
- PURPOSE
To describe our initial experience with the second-generation Single Port Instrument Delivery Extended Reach (SPIDER) laparoendoscopic single-site surgical system in a porcine model.
MATERIALS AND METHODS
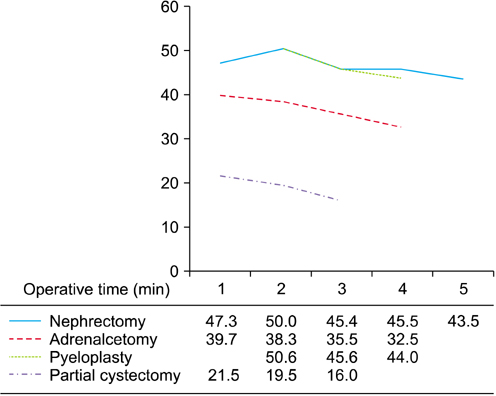
In four swine weighing approximately 32 to 35 kg, five nephrectomies, four adrenalectomies, three pyeloplasties, and three partial cystectomies and closures were performed by a single surgeon. The swine were placed in the lateral flank position under general anesthesia. The SPIDER surgical system was introduced through a single incision and the various urological procures were performed by use of flexible instrumentation.
RESULTS
All five nephrectomies, four adrenalectomies, three pyeloplasties, and three partial cystectomies and closures were performed successfully without additional skin incisions. The mean time to set up the SPIDER platform was 3.5 minutes. The mean operative time for the right and left nephrectomies was 45.4 minutes and 47.8 minutes, respectively. The mean operative time for the right and left adrenalectomies was 37.6 minutes and 35.4 minutes, respectively. The mean operative time for the pyeloplasties for one right and two left ureters was 45.6 minutes and 47.3 minutes, respectively. The mean operative time for the partial cystectomies and closures was 18.6 minutes. There were no noticeable intraoperative complications except for minimal urine leakage in the first pyeloplasty.
CONCLUSIONS
In this initial pilot evaluation, the second-generation SPIDER surgical system offered intuitive instrument maneuverability and restored triangulation. However, retraction was challenging because of the lack of strength and the limited ability for precise manipulation of the tip. Future refinements of the technology and prospective studies are needed to optimize the application of this technology in urology.
Keyword
MeSH Terms
Figure
Reference
-
1. Gettman MT, Lotan Y, Napper CA, Cadeddu JA. Transvaginal laparoscopic nephrectomy: development and feasibility in the porcine model. Urology. 2002. 59:446–450.2. Gettman MT, Box G, Averch T, Cadeddu JA, Cherullo E, Clayman RV, et al. Consensus statement on natural orifice transluminal endoscopic surgery and single-incision laparoscopic surgery: heralding a new era in urology? Eur Urol. 2008. 53:1117–1120.3. Autorino R, Cadeddu JA, Desai MM, Gettman M, Gill IS, Kavoussi LR, et al. Laparoendoscopic single-site and natural orifice transluminal endoscopic surgery in urology: a critical analysis of the literature. Eur Urol. 2011. 59:26–45.4. Kaouk JH, Autorino R, Kim FJ, Han DH, Lee SW, Yinghao S, et al. Laparoendoscopic single-site surgery in urology: worldwide multi-institutional analysis of 1076 cases. Eur Urol. 2011. 60:998–1005.5. Tracy CR, Raman JD, Cadeddu JA, Rane A. Laparoendoscopic single-site surgery in urology: where have we been and where are we heading? Nat Clin Pract Urol. 2008. 5:561–568.6. Tugcu V, Ilbey YO, Mutlu B, Tasci AI. Laparoendoscopic single-site surgery versus standard laparoscopic simple nephrectomy: a prospective randomized study. J Endourol. 2010. 24:1315–1320.7. Andonian S, Rais-Bahrami S, Atalla MA, Herati AS, Richstone L, Kavoussi LR. Laparoendoscopic single-site Pfannenstiel versus standard laparoscopic donor nephrectomy. J Endourol. 2010. 24:429–432.8. Tracy CR, Raman JD, Bagrodia A, Cadeddu JA. Perioperative outcomes in patients undergoing conventional laparoscopic versus laparoendoscopic single-site pyeloplasty. Urology. 2009. 74:1029–1034.9. Jeong BC, Park YH, Han DH, Kim HH. Laparoendoscopic single-site and conventional laparoscopic adrenalectomy: a matched case-control study. J Endourol. 2009. 23:1957–1960.10. White WM, Goel RK, Kaouk JH. Single-port laparoscopic retroperitoneal surgery: initial operative experience and comparative outcomes. Urology. 2009. 73:1279–1282.11. White WM, Goel RK, Swartz MA, Moore C, Rackley RR, Kaouk JH. Single-port laparoscopic abdominal sacral colpopexy: initial experience and comparative outcomes. Urology. 2009. 74:1008–1012.12. Stolzenburg JU, Kallidonis P, Oh MA, Ghulam N, Do M, Haefner T, et al. Comparative assessment of laparoscopic single-site surgery instruments to conventional laparoscopic in laboratory setting. J Endourol. 2010. 24:239–245.13. Irwin BH, Rao PP, Stein RJ, Desai MM. Laparoendoscopic single site surgery in urology. Urol Clin North Am. 2009. 36:223–235. ix14. de la Fuente SG, Demaria EJ, Reynolds JD, Portenier DD, Pryor AD. New developments in surgery: Natural Orifice Transluminal Endoscopic Surgery (NOTES). Arch Surg. 2007. 142:295–297.15. Rattner D, Kalloo A. ASGE/SAGES Working Group. ASGE/SAGES Working Group on Natural Orifice Translumenal Endoscopic Surgery. October 2005. Surg Endosc. 2006. 20:329–333.16. Desai MM, Berger AK, Brandina R, Aron M, Irwin BH, Canes D, et al. Laparoendoscopic single-site surgery: initial hundred patients. Urology. 2009. 74:805–812.17. White WM, Haber GP, Goel RK, Crouzet S, Stein RJ, Kaouk JH. Single-port urological surgery: single-center experience with the first 100 cases. Urology. 2009. 74:801–804.18. Raman JD, Bagrodia A, Cadeddu JA. Single-incision, umbilical laparoscopic versus conventional laparoscopic nephrectomy: a comparison of perioperative outcomes and short-term measures of convalescence. Eur Urol. 2009. 55:1198–1204.19. Raybourn JH 3rd, Rane A, Sundaram CP. Laparoendoscopic single-site surgery for nephrectomy as a feasible alternative to traditional laparoscopy. Urology. 2010. 75:100–103.20. Choi KH, Ham WS, Rha KH, Lee JW, Jeon HG, Arkoncel FR, et al. Laparoendoscopic single-site surgeries: a single-center experience of 171 consecutive cases. Korean J Urol. 2011. 52:31–38.21. Autorino R, Haber GP, White MA, Khanna R, Altunrende F, Yang B, et al. Pure and hybrid natural orifice transluminal endoscopic surgery (NOTES): current clinical experience in urology. BJU Int. 2010. 106(6 Pt B):919–922.22. Gill IS, Canes D, Aron M, Haber GP, Goldfarb DA, Flechner S, et al. Single port transumbilical (E-NOTES) donor nephrectomy. J Urol. 2008. 180:637–641.23. Desai MM, Stein R, Rao P, Canes D, Aron M, Rao PP, et al. Embryonic natural orifice transumbilical endoscopic surgery (E-NOTES) for advanced reconstruction: initial experience. Urology. 2009. 73:182–187.24. Pryor AD, Tushar JR, DiBernardo LR. Single-port cholecystectomy with the TransEnterix SPIDER: simple and safe. Surg Endosc. 2010. 24:917–923.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Robot-assisted laparoendoscopic single-site upper urinary tract surgery with da Vinci Xi surgical system: Initial experience
- Concomitant Laparoendoscopic Single-Site Surgery for Vesicolithotomy and Finger-Assisted Single-Port Transvesical Enucleation of the Prostate
- Hybrid laparoscopic myomectomy: A novel technique
- A Case of Single Port Laparoscopic Appendectomy and Cholecystectomy in a Fresh Cadaver: A Feasible Procedure
- Single port laparoscopic surgery