Clin Endosc.
2014 Mar;47(2):201-204. 10.5946/ce.2014.47.2.201.
A Case of Choledocholithiasis and Intestinal Malrotation in an Adolescent with Repaired Gastroschisis
- Affiliations
-
- 1Department of Internal Medicine, Chungbuk National University College of Medicine, Cheongju, Korea. smpark@chungbuk.ac.kr
- KMID: 2049011
- DOI: http://doi.org/10.5946/ce.2014.47.2.201
Abstract
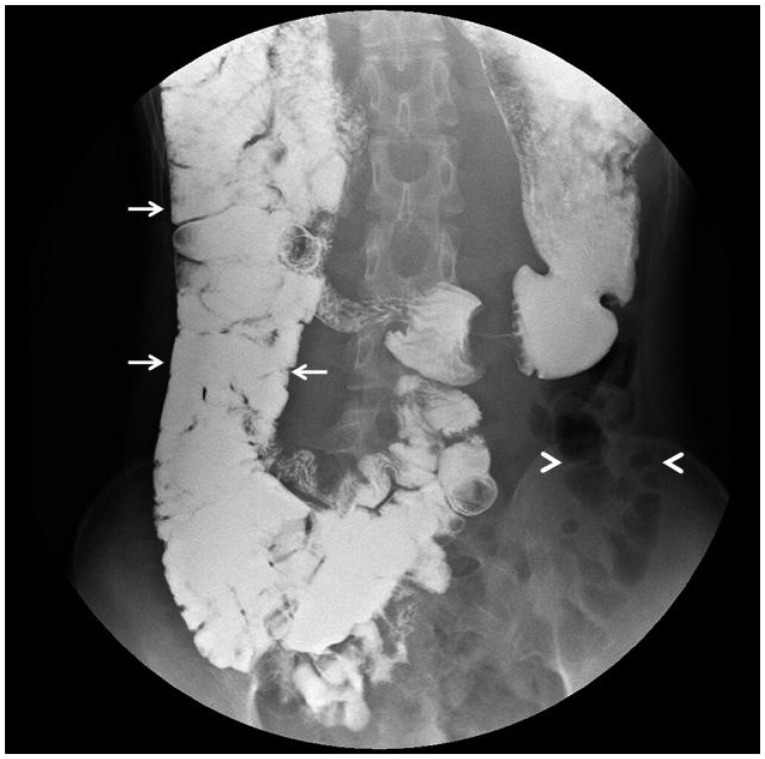
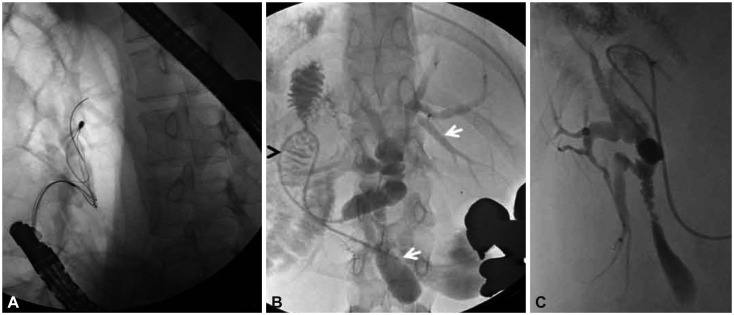
- Most infants with repaired gastroschisis develop normally and remain in good health. About 10% of patients with gastroschisis have other malformations. We report a case of choledocholithiasis and intestinal malrotation in an adolescent with repaired gastroschisis. A 17-year-old girl presented with fever, jaundice, and abdominal pain. She had undergone an operation to repair gastroschisis at birth. Physical examination revealed icteric sclera, a tight abdominal wall, and a longitudinal surgical scar at the midline. An abdominal computed tomography scan revealed a round calcifying lesion near the pancreas and a midline-positioned liver and gallbladder. Absence of the retroperitoneal duodenum and the anterior and left-sided position of the superior mesenteric vein compared with the superior mesenteric artery were observed. Results of abarium examination revealed intestinal malrotation. Endoscopic retrograde cholangiopancreatography revealed diffuse dilatation of the biliary trees and a malpositioned gallbladder. A single stone was removed by using a basket. The clinical symptoms improved after the patient underwent endoscopic retrograde cholangiopancreatography.
MeSH Terms
Figure
Reference
-
1. Hunter AG, Stevenson RE. Gastroschisis: clinical presentation and associations. Am J Med Genet C Semin Med Genet. 2008; 148C:219–230. PMID: 18655099.
Article2. Tunell WP, Puffinbarger NK, Tuggle DW, Taylor DV, Mantor PC. Abdominal wall defects in infants. Survival and implications for adult life. Ann Surg. 1995; 221:525–528. PMID: 7748034.
Article3. Islam S. Clinical care outcomes in abdominal wall defects. Curr Opin Pediatr. 2008; 20:305–310. PMID: 18475100.
Article4. Davies BW, Stringer MD. The survivors of gastroschisis. Arch Dis Child. 1997; 77:158–160. PMID: 9301359.
Article5. Serber J, Stranzinger E, Geiger JD, Teitelbaum DH. Association of gastroschisis and choledochal cyst. J Pediatr Surg. 2009; 44:e23–e26. PMID: 19302840.
Article6. Lee TC, Barshes NR, Nguyen L, et al. Gastroschisis and biliary atresia in a neonate: uncommon presentation or common precipitant. Eur J Pediatr Surg. 2005; 15:434–436. PMID: 16418964.
Article7. Teoh L, Wong CK, Martin H, O'Loughlin EV. Anterior abdominal wall defects and biliary obstruction. J Paediatr Child Health. 2005; 41:143–146. PMID: 15790327.
Article8. Hancock BJ, Wiseman NE, Rusnak BW. Bile duct stricture in an infant with gastroschisis treated by percutaneous transhepatic drainage, biliary stenting, and balloon dilation. J Pediatr Surg. 1989; 24:1071–1073. PMID: 2530328.
Article9. Daneman A. Malrotation: the balance of evidence. Pediatr Radiol. 2009; 39(Suppl 2):S164–S166. PMID: 19308379.
Article10. Loyer E, Eggli KD. Sonographic evaluation of superior mesenteric vascular relationship in malrotation. Pediatr Radiol. 1989; 19:173–175. PMID: 2654854.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Left Sided Appendicitis in Patient with Intestinal Malrotation
- A Case of Duodenal Web Associated with Intestinal Malrotation
- Fetal Surgery: Gastroschisis Model in Rabbits
- Malrotation complicating Midgut Volvulus: Ultrasonographic Finding
- Various Imaging Features of Intestinal Malrotation, Associated Anomalies, and Complications