J Korean Surg Soc.
2010 Dec;79(Suppl 1):S31-S36. 10.4174/jkss.2010.79.Suppl1.S31.
Gastric Outlet Obstruction due to Submucosal Neurofibromatous Proliferation of Duodenal Bulb in Neurofibromatosis Type 1 Patient
- Affiliations
-
- 1Department of Surgery, Pundang Jesaeng General Hospital, Daejin Medical Center, Seongnam, Korea. bssuhgs@empas.com
- 2Department of Pathology, Pundang Jesaeng General Hospital, Daejin Medical Center, Seongnam, Korea.
- 3Division of Gastroenterology, Pundang Jesaeng General Hospital, Daejin Medical Center, Seongnam, Korea.
- KMID: 2040549
- DOI: http://doi.org/10.4174/jkss.2010.79.Suppl1.S31
Abstract
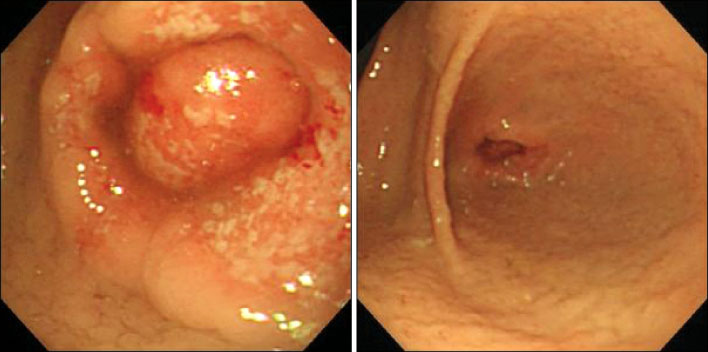
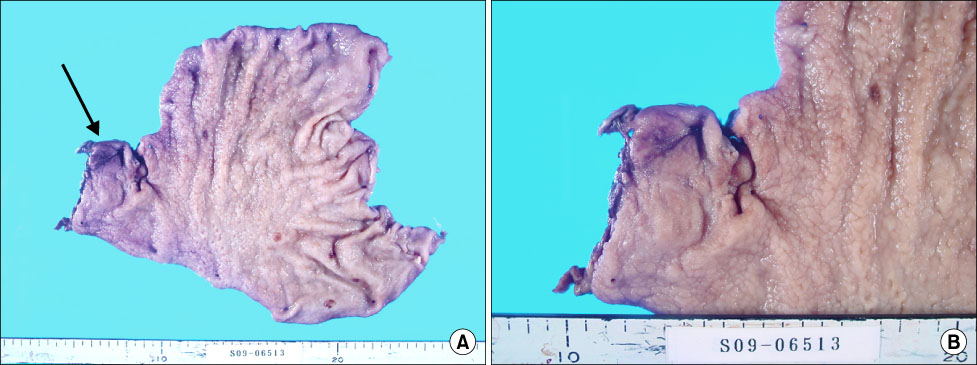
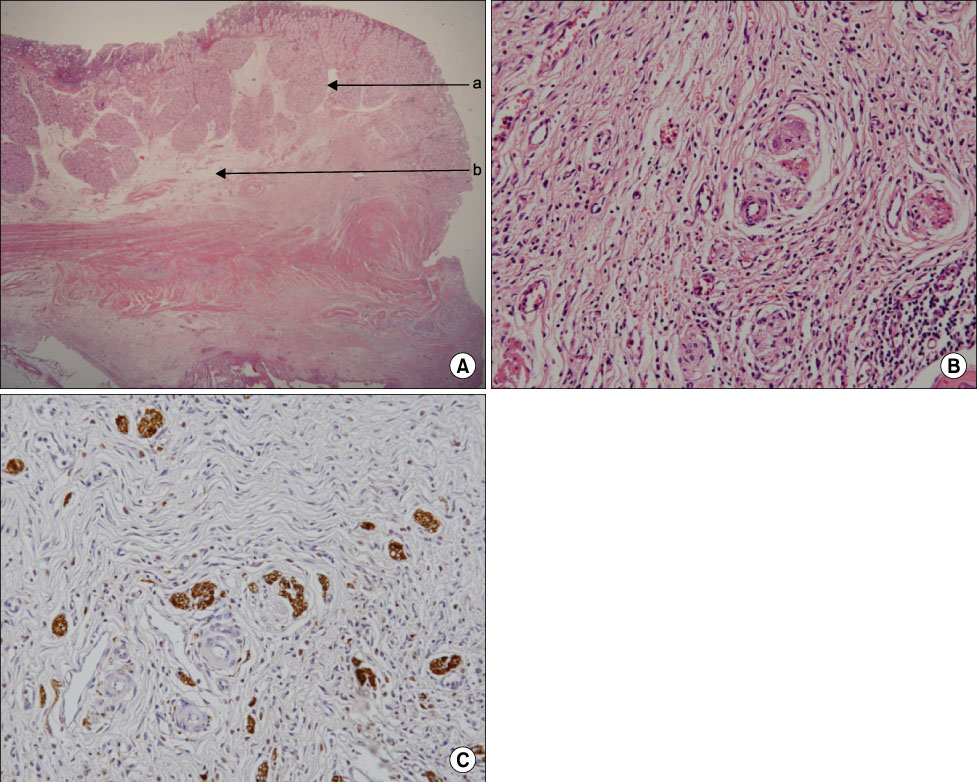
- Neurofibromatosis type 1 (NF1; also known as von Recklinghausen's neurofibromatosis) is inherited in an autosomal dominant fashion, although it can also arise due to spontaneous mutation. Gastrointestinal involvement of NF1 is seen in 10% to 25% and causes symptoms in fewer than 5%. Histologically, the gastro intestinal (GI) manifestation of NF1 occurs in three forms: hyperplasia of the gut neural tissue, stromal tumors, and duodenal or periampullary endocrine tumors. A 31-year-old female, diagnosed with NF1, presented with poor oral intake and vomiting for 10 days prior to admission. Preoperative gastrofiberscopic finding was gastric outlet obstructing polypoid duodenal bulb lesion. The patient underwent hemigastrectomy with antecolic gastrojejunostomy due to gastric outlet obstruction. The final pathologic report was submucosal neurofibromatous proliferation with Brunner's gland hyperplasia located at the duodenal bulb in the NF1 patient. We report this case with a review of literatures.
MeSH Terms
Figure
Reference
-
1. Sergeyev AS. On the mutation rate of neurofibromatosis. Humangenetik. 1975. 28:129–138.2. Barker D, Wright E, Nguyen K, Cannon L, Fain P, Goldgar D, et al. Gene for von Recklinghausen neurofibromatosis is in the polycentromeric region of chromosome 17. Science. 1987. 236:1100–1102.3. Seizinger BR, Rouleau GA, Ozelius LJ, Lane AH, Faryniarz AG, Chao MV, et al. Genetic linkage of von Recklinghausen neurofibromatosis to the nerve growth factor receptor gene. Cell. 1987. 49:589–594.4. Riccardi VM. Von Recklinghausen neurofibromatosis. N Engl J Med. 1981. 305:1617–1627.5. Huson SM, Harper PS, Compston DA. Von Recklinghausen neurofibromatosis. A clinical and population study in southeast Wales. Brain. 1988. 111(Pt 6):1355–1381.6. Fuller CE, Williams GT. Gastrointestinal manifestations of type 1 neurofibromatosis (von Recklinghausen's disease). Histopathology. 1991. 19:1–11.7. Seymour-Dempsey K, Andrassy RJ. Neurofibromatosis: implications for the general surgeon. J Am Coll Surg. 2002. 195:553–563.8. Phat VN, Sezeur A, Danne M, Dupuis D, de la Vaissiere G, Camilleri JP. Primary myenteric plexus alterations as a cause of megacolon in Von Recklinghausen's disease. Pathol Biol (Paris). 1980. 28:585–588.9. Fenoglio-Preiser CM. Gastrointestinal Pathology: An Atlas and Text. 2008. 3rd ed. Philadelphia: Lippincott Williams & Wilkins.10. Bakker JR, Haber MM, Garcia FU. Gastrointestinal neurofibromatosis: an unusual cause of gastric outlet obstruction. Am Surg. 2005. 71:100–105.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Gastric Outlet Obstruction by Impacted Phytobezoar at the Normal Duodenal Bulb
- Successful Endoscopic Decompression for Intramural Duodenal Hematoma with Gastric Outlet Obstruction Complicating Acute Pancreatitis
- A Case of Polypoid Gastric Metaplasia in Duodenal Bulb
- Endoscopic Management of Combined Biliary and Duodenal Obstruction
- Clinicopathologic Analysis of Gastric Carcinoma Patients with Outlet Obstruction