J Periodontal Implant Sci.
2013 Aug;43(4):160-167. 10.5051/jpis.2013.43.4.160.
An analysis on the factors responsible for relative position of interproximal papilla in healthy subjects
- Affiliations
-
- 1Department of Periodontology, Pusan National University School of Dentistry, Yangsan, Korea. kimjh1227@naver.com
- KMID: 2027811
- DOI: http://doi.org/10.5051/jpis.2013.43.4.160
Abstract
- PURPOSE
This study examined the factors that can be associated with the appearance of the interproximal papilla.
METHODS
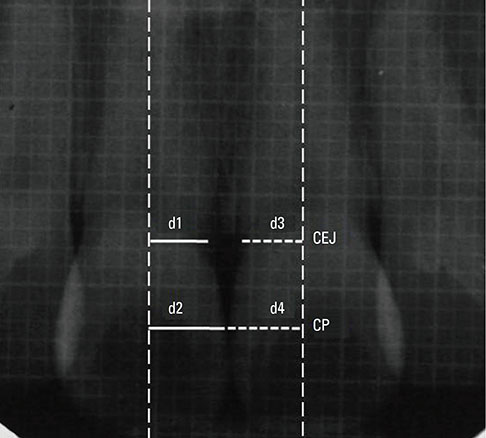
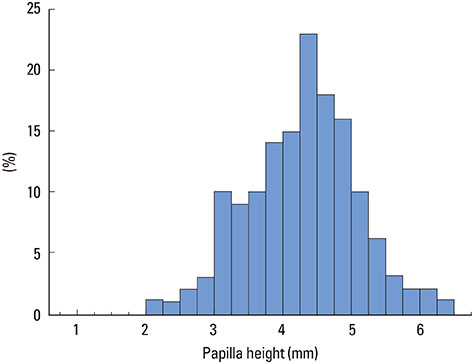
One hundred and forty-seven healthy interproximal papillae between the maxillary central incisors were examined. For each subject, a digital photograph and periapical radiograph of the interdental embrasure were taken using a 1-mm grid metal piece. The following parameters were recorded: the amount of recession of the interproximal papilla, contact point-bone crest distance, contact point-cemento-enamel junction (CEJ) distance, CEJ-bone crest distance, inter-radicular distance, tooth shape, embrasure space size, interproximal contact area, gingival biotype, papilla height, and papilla tip form.
RESULTS
The amount of recession of the interproximal papilla was associated with the following: 1) increase in contact point-bone crest, contact point-CEJ, and CEJ-bone crest distance; 2) increase in the inter-radicular distance; 3) triangular tooth shape; 4) decrease in the interproximal contact area length; 5) increase in the embrasure space size; and 6) flat papilla tip form. On the other hand, the amount of gingival recession was not associated with the gingival biotype or papilla height. In the triangular tooth shape, the contact point-bone crest distance and inter-radicular distance were longer, the interproximal contact area length was shorter, and the embrasure space size was larger. The papilla tip form became flatter with increasing inter-radicular distance and CEJ-bone crest distance.
CONCLUSIONS
The relative position of the interproximal papilla in healthy subjects was associated with the multiple factors and each factor was related to the others. A triangular tooth shape carries a higher risk of recession of the interproximal papilla because the proximal contact point is positioned more incisally and the bone crest is positioned more apically. This results in an increase in recession of the interproximal papilla and flat papilla tip form.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The association between radiographic embrasure morphology and interdental papilla reconstruction using injectable hyaluronic acid gel
Won-Pyo Lee, Yo-Seob Seo, Hee-Jung Kim, Sang-Joun Yu, Byung-Ock Kim
J Periodontal Implant Sci. 2016;46(4):277-287. doi: 10.5051/jpis.2016.46.4.277.
Reference
-
1. An KY, Lee JY, Kim SJ, Choi JI. Perception of maxillary anterior esthetics by dental professionals and laypeople and survey of gingival topography in healthy young subjects. Int J Periodontics Restorative Dent. 2009; 29:535–541.2. Moskowitz ME, Nayyar A. Determinants of dental esthetics: a rational for smile analysis and treatment. Compend Contin Educ Dent. 1995; 16:1164. 1166.3. Zetu L, Wang HL. Management of inter-dental/inter-implant papilla. J Clin Periodontol. 2005; 32:831–839.
Article4. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992; 63:995–996.
Article5. Kokich V. Adjunctive Role of Orthodontic Therapy. In : Newman MG, Takei HH, Klokkevold PR, Carranza FA, editors. Carranza's clinical periodontology. 10th ed. Philadelphia: WB Saunders;2006. p. 856–870.6. Chow YC, Eber RM, Tsao YP, Shotwell JL, Wang HL. Factors associated with the appearance of gingival papillae. J Clin Periodontol. 2010; 37:719–727.
Article7. Chen MC, Liao YF, Chan CP, Ku YC, Pan WL, Tu YK. Factors influencing the presence of interproximal dental papillae between maxillary anterior teeth. J Periodontol. 2010; 81:318–324.
Article8. Chang LC. Assessment of parameters affecting the presence of the central papilla using a non-invasive radiographic method. J Periodontol. 2008; 79:603–609.
Article9. Cho HS, Jang HS, Kim DK, Park JC, Kim HJ, Choi SH, et al. The effects of interproximal distance between roots on the existence of interdental papillae according to the distance from the contact point to the alveolar crest. J Periodontol. 2006; 77:1651–1657.
Article10. Sasaki T, Mizuno S, Matsui T. The height of interdental papilla and interradicular distance in healthy periodontium. Quintessence. 2010; 15:120–128.11. Sasaki T, Mizuno S, Matsui T. Reconstruction of interdental papilla after apically positioned flap. Quintessence. 2010; 15:96–103.12. Kois JC. Predictable single-tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2004; 25:895–896. 89890013. Kurth JR, Kokich VG. Open gingival embrasures after orthodontic treatment in adults: prevalence and etiology. Am J Orthod Dentofacial Orthop. 2001; 120:116–123.
Article14. Morris ML. The position of the margin of the gingiva. Oral Surg Oral Med Oral Pathol. 1958; 11:969–984.
Article15. Wheeler RC. Complete crown form and the periodontium. J Prosthet Dent. 1961; 11:722–734.
Article16. Shigeno K. Understand Periodontal Plastic Surgery. In : Shigeno K, editor. Illustrated periodontal plastic surgery. Toyko: Ishiyaku Publishers;2005. p. 290–331.17. Ochsenbein C, Ross S. A reevaluation of osseous surgery. Dent Clin North Am. 1969; 13:87–102.18. Seibert J, Lindhe J. Esthetics and Periodontal Therapy. In : Lindhe J, editor. Textbook of clinical periodontology. 2nd ed. Copenhangen: Munksgaard;1989. p. 477–514.19. Maynard JG Jr, Wilson RD. Physiologic dimensions of the periodontium significant to the restorative dentist. J Periodontol. 1979; 50:170–174.
Article20. Kumari BN, Thiagarajan R, Narayanan V, Devadoss P, Mammen B, Emmadi P. A new technique for root coverage using buccal fat pad: a short case report. Quintessence Int. 2010; 41:547–549.21. Moskow BS, Tannenbaum P, Bloom A. Visualization of the human periodontium using serial thin section contact radiography. J Periodontol. 1985; 56:223–233.
Article22. Spear FM. Maintenance of the interdental papilla following anterior tooth removal. Pract Periodontics Aesthet Dent. 1999; 11:21–28.23. Olsson M, Lindhe J, Marinello CP. On the relationship between crown form and clinical features of the gingiva in adolescents. J Clin Periodontol. 1993; 20:570–577.
Article24. Claffey N, Shanley D. Relationship of gingival thickness and bleeding to loss of probing attachment in shallow sites following nonsurgical periodontal therapy. J Clin Periodontol. 1986; 13:654–657.
Article25. Fu JH, Yeh CY, Chan HL, Tatarakis N, Leong DJ, Wang HL. Tissue biotype and its relation to the underlying bone morphology. J Periodontol. 2010; 81:569–574.
Article26. Müller HP, Schaller N, Eger T. Ultrasonic determination of thickness of masticatory mucosa: a methodologic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 88:248–253.
Article27. Kan JY, Morimoto T, Rungcharassaeng K, Roe P, Smith DH. Gingival biotype assessment in the esthetic zone: visual versus direct measurement. Int J Periodontics Restorative Dent. 2010; 30:237–243.28. Sanavi F, Weisgold AS, Rose LF. Biologic width and its relation to periodontal biotypes. J Esthet Dent. 1998; 10:157–163.
Article29. Olsson M, Lindhe J. Periodontal characteristics in individuals with varying form of the upper central incisors. J Clin Periodontol. 1991; 18:78–82.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of slow forced eruption on the vertical levels of the interproximal bone and papilla and the width of the alveolar ridge
- Effect of interproximal undercut on the dimensional accuracy of impression
- Relationship between Interdental Papilla Existence & Distance from Interdental Alveolar Crest to Contact Point in the Posterior Dentition of Korean adults
- A Relationship between Interdental Papilla Existence and the Distance from Contact Point to Interdental Alveolar Crest in the Maxillary Anterior Dentition of Korean adults
- Effect of immediate provisional restoration on the preservation of gingival contour