J Korean Neurosurg Soc.
2014 May;55(5):261-266. 10.3340/jkns.2014.55.5.261.
A Morphometric Study of the Lumbar Interspinous Space in 100 Stanford University Medical Center Patients
- Affiliations
-
- 1Department of Neurosurgery, Kangwon National University School of Medicine, Chuncheon, Korea. nsped@kangwon.ac.kr
- KMID: 2018031
- DOI: http://doi.org/10.3340/jkns.2014.55.5.261
Abstract
OBJECTIVE
With the increased use of interspinous spacers in the treatment of lumbar stenosis, knowledge of the geometry of the interspinous space is important. To prevent dislodgment of an interspinous spacer, the accurate depth and width of the interspinous space needs to be established to facilitate the best intraoperative selection of correct spacer size.
METHODS
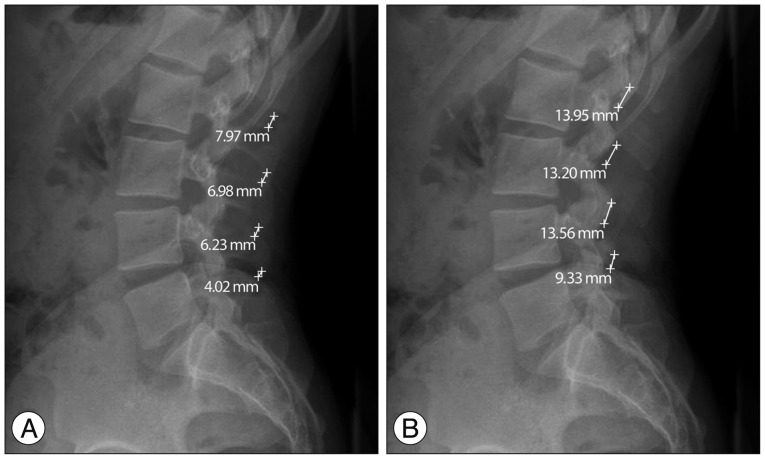
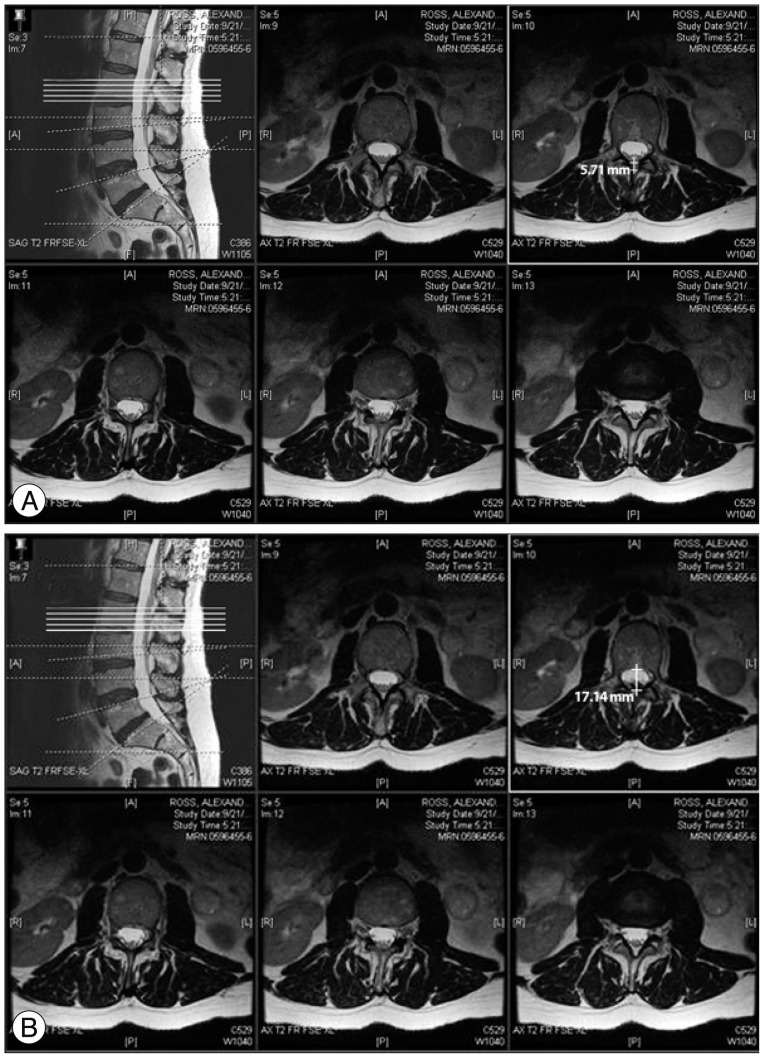
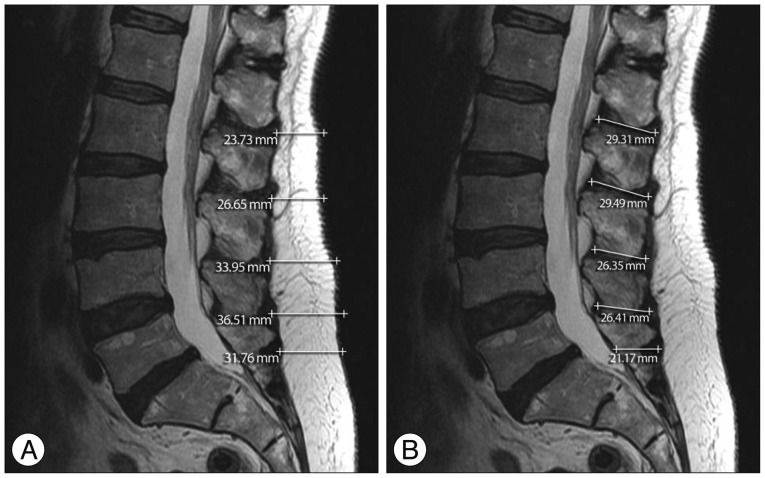
To determine the depth and width of the interspinous space, two methods are available which utilize plain film and magnetic resonance imaging (MRI). Data analysis of the interspinous depth and width was undertaken in 100 patients.
RESULTS
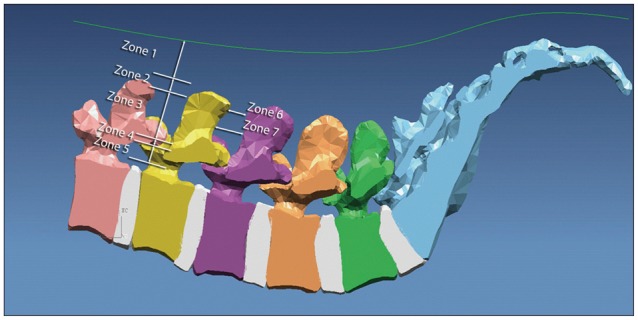
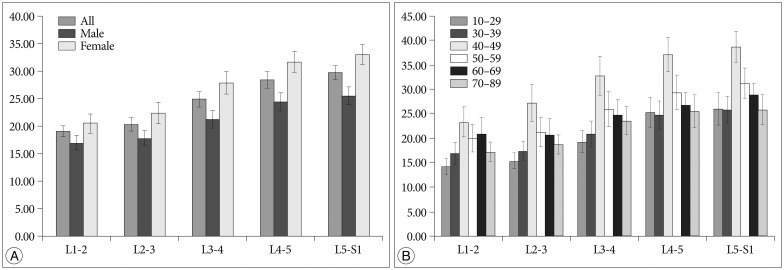
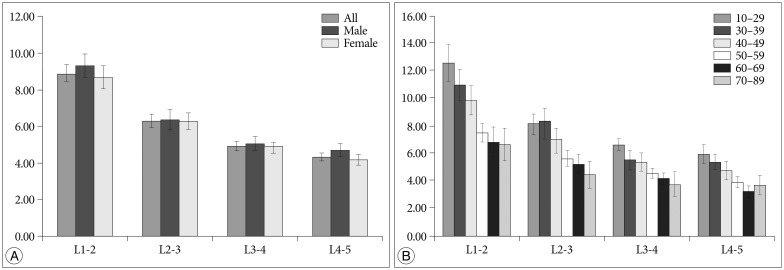
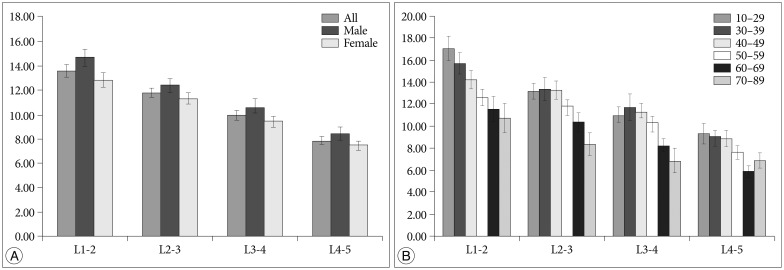
The standard deviations were variable, since skin thickness (zone 1) was altered by sex and age. The difference in the zone 1 distance between adjacent interspinous processes varied according to gender (p<0.05), but was not influenced by age [p=0.32 by analysis of variance between groups (ANOVA)]. Zone 2, the supraspinous, and zone 3, the interspinous ligament depths, comprise the operative working area during insertion of an interspinous spacer. There were no differences with regard to gender or age (p>0.05). For zones 6 and 7, the interspinous distances at the narrowest and widest points, respectively, were found to decrease with the aging process, but the decrease was not statistically significant. There were no differences with regard to gender (p>0.05).
CONCLUSION
This study provides additional information on the interspinous space. This statistical data are valuable for use in the design of interspinous spacers.
Keyword
MeSH Terms
Figure
Reference
-
1. Andersson GB, Schultz A, Nathan A, Irstam L. Roentgenographic measurement of lumbar intervertebral disc height. Spine (Phila Pa 1976). 1981; 6:154–158. PMID: 7280816.
Article2. Gilad I, Nissan M. A study of vertebra and disc geometric relations of the human cervical and lumbar spine. Spine (Phila Pa 1976). 1986; 11:154–157. PMID: 3704802.
Article3. Hayes MA, Howard TC, Gruel CR, Kopta JA. Roentgenographic evaluation of lumbar spine flexion-extension in asymptomatic individuals. Spine (Phila Pa 1976). 1989; 14:327–331. PMID: 2711247.
Article4. Johnson GM, Zhang M. Regional differences within the human supraspinous and interspinous ligaments : a sheet plastination study. Eur Spine J. 2002; 11:382–388. PMID: 12194001.
Article5. Neumann P, Wang Y, Kärrholm J, Malchau H, Nordwall A. Determination of inter-spinous process distance in the lumbar spine. Evaluation of reference population to facilitate detection of severe trauma. Eur Spine J. 1999; 8:272–278. PMID: 10483828.6. Nissan M, Gilad I. Dimensions of human lumbar vertebrae in the sagittal plane. J Biomech. 1986; 19:753–758. PMID: 3793749.
Article7. Nissan M, Gilad I. The cervical and lumbar vertebrae-an anthropometric model. Eng Med. 1984; 13:111–114. PMID: 6542880.8. Panjabi MM, Greenstein G, Duranceau J, Nolte LP. Three-dimensional quantitative morphology of lumbar spinal ligaments. J Spinal Disord. 1991; 4:54–62. PMID: 1807531.9. Pope MH, Hanley EN, Matteri RE, Wilder DG, Frymoyer JW. Measurement of intervertebral disc space height. Spine. 1977; 2:282–286.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Utility of an Imaginary Line between the Both Posterior Superior Iliac Spines for Judgement of L4-5 Interspinous Space
- Preliminary Report on Usefulness of Adjacent Interspinous Stabilization using Interspinous Spacer Combined with Posterior Lumbosacral Spinal Fusion in Degenerative Lumbar Disease
- ASCO 2019 meeting review
- Long-term Follow-up (Minimum 5 Years) Study of Single-level Posterior Dynamic Stabilization in Lumbar Degenerative Disease; 'Interspinous U' & 'DIAM'
- Real world adverse events of interspinous spacers using Manufacturer and User Facility Device Experience data