J Korean Soc Radiol.
2010 May;62(5):457-460. 10.3348/jksr.2010.62.5.457.
A Posterior Mediastinal Seminoma with Extensive Cystic Change
- Affiliations
-
- 1Department of Radiology, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine, Korea. ksbae@gnu.ac.kr
- 2Department of Pathology, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine, Korea.
- 3Department of Thoracic Surgery, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine, Korea.
- KMID: 2002953
- DOI: http://doi.org/10.3348/jksr.2010.62.5.457
Abstract
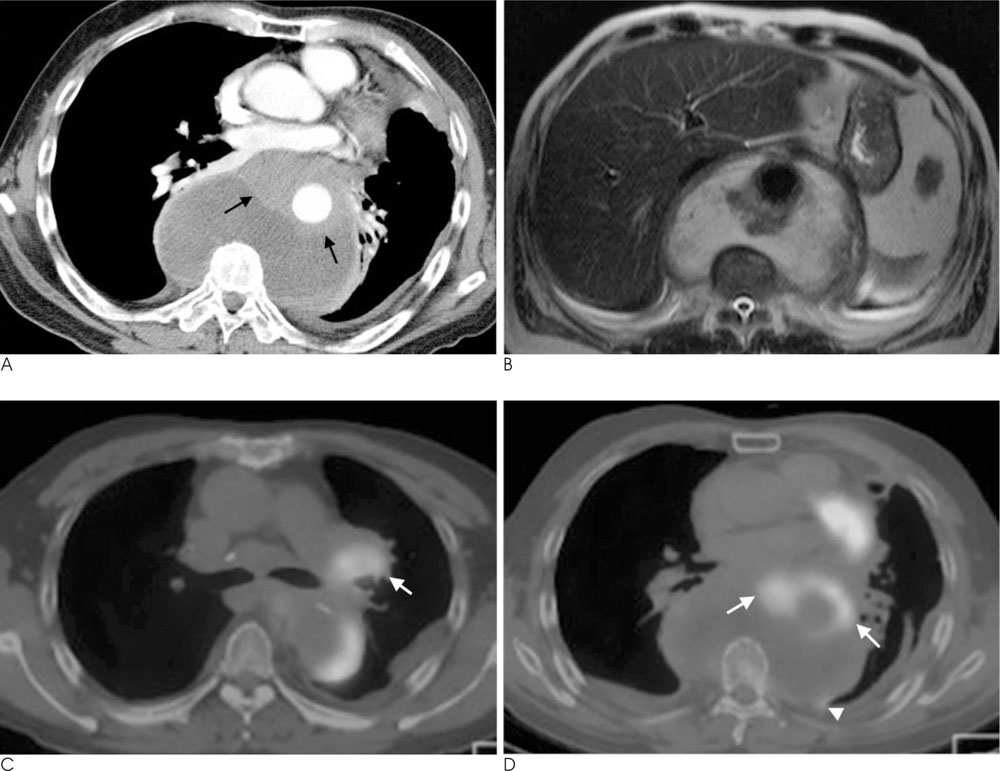
- The posterior mediastinum is a rare site of origin for seminoma, and extensive cystic change of a seminoma is rarely observed. We present here the case of a 62-year-old male patient with a primary posterior mediastinal seminoma that was encasing the descending thoracic aorta and the tumor showed prominent cystic change on CT and MRI, and intense FDG uptake on PET/CT.
MeSH Terms
Figure
Reference
-
1. Moran CA, Suster S, Przygodzki RM, Koss MN. Primary germ cell tumors of the mediastinum: II. Mediastinal seminomas -- a clinicopathologic and immunohistochemical study of 120 cases. Cancer. 1997; 80:691–698.2. Luna MA, Valenzuela-Tamariz J. Germ-cell tumors of the mediastinum, postmortem findings. Am J Clin Pathol. 1976; 65:450–454.3. Ravenel JG, Gordon LL, Block MI, Chaudhary U. Primary posterior mediastinal seminoma. AJR Am J Roentgenol. 2004; 183:1835–1837.4. Rosado-de-Christenson ML, Templeton PA, Moran CA. From the archives of the AFIP. Mediastinal germ cell tumors: radiologic and pathologic correlation. Radiographics. 1992; 12:1013–1030.5. Makiyama K, Senga Y. Primary seminoma in the posterior mediastinum. J Urol. 2001; 165:908.6. Bokemeyer C, Droz JP, Horwich A, Gerl A, Fossa SD, Beyer J, et al. Extragonadal seminoma: an international multicenter analysis of prognostic factors and long term treatment outcome. Cancer. 2001; 91:1394–1401.7. Johnson JO, Mattrey RF, Phillipson J. Differentiation of seminomatous from nonseminomatous testicular tumors with MR imaging. AJR Am J Roentgenol. 1990; 154:539–543.8. Flynn MJ, Childerhouse A, Mead GM, Theaker JM. Unusual cystic change in classic seminoma of the testis. Am J Surg Pathol. 2006; 30:137–139.9. Moran CA, Suster S. Mediastinal seminomas with prominent cystic changes. A clinicopathologic study of 10 cases. Am J Surg Pathol. 1995; 19:1047–1053.10. Kurosaki Y, Tanaka YO, Itai Y. Thymic seminoma with prominent cystic changes. AJR Am J Roentgenol. 1996; 167:1345–1346.