J Korean Soc Radiol.
2013 Nov;69(5):361-364. 10.3348/jksr.2013.69.5.361.
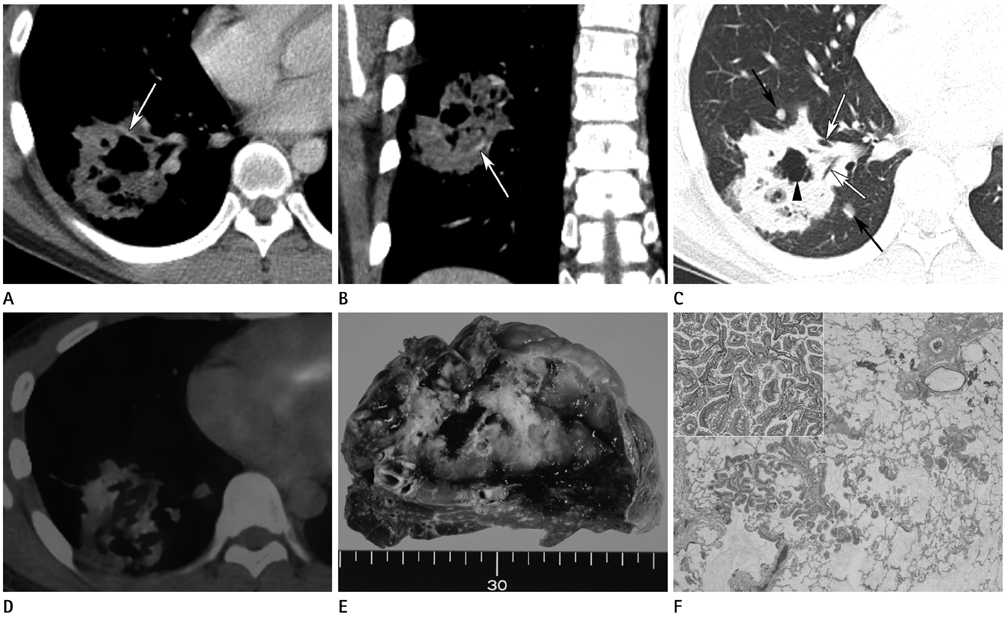
Pulmonary Invasive Mucinous Adenocarcinoma in an Asymptomatic 23-Year-Old Male: Presentation with a Large Cavitary Mass
- Affiliations
-
- 1Department of Radiology, Chonnam National University Hospital, Gwangju, Korea. seonhj@jnu.ac.kr
- 2Department of Radiology, Chonnam National University Hwasun Hospital, Hwasun, Korea.
- 3Department of Pathology, Chonnam National University Medical School, Gwangju, Korea.
- 4Department of Thoracic and Cardiovascular Surgery, Chonnam National University Medical School, Gwangju, Korea.
- KMID: 2002856
- DOI: http://doi.org/10.3348/jksr.2013.69.5.361
Abstract
- Pulmonary invasive mucinous adenocarcinoma (PIMA) formerly known as mucinous bronchioalveolar carcinoma is a relatively rare variant of pulmonary adenocarcinoma, but the incidence of this tumor is known to be rising. Imaging findings may include nodules, masses and lobar involvement of variable densities, but the majority present as air-space consolidation. We report a case of PIMA with radiological-pathological correlation in a 23-year-old male which presented as a large cavitary mass mimicking congenital cystic lung disease.
MeSH Terms
Figure
Reference
-
1. Travis WD, Brambilla E, Noguchi M, Nicholson AG, Geisinger KR, Yatabe Y, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol. 2011; 6:244–285.2. Lee KS, Kim Y, Han J, Ko EJ, Park CK, Primack SL. Bronchioloalveolar carcinoma: clinical, histopathologic, and radiologic findings. Radiographics. 1997; 17:1345–1357.3. Austin JH, Garg K, Aberle D, Yankelevitz D, Kuriyama K, Lee HJ, et al. Radiologic implications of the 2011 classification of adenocarcinoma of the lung. Radiology. 2013; 266:62–71.4. Akira M, Atagi S, Kawahara M, Iuchi K, Johkoh T. High-resolution CT findings of diffuse bronchioloalveolar carcinoma in 38 patients. AJR Am J Roentgenol. 1999; 173:1623–1629.5. Patsios D, Roberts HC, Paul NS, Chung T, Herman SJ, Pereira A, et al. Pictorial review of the many faces of bronchioloalveolar cell carcinoma. Br J Radiol. 2007; 80:1015–1023.6. Beasley MB, Brambilla E, Travis WD. The 2004 World Health Organization classification of lung tumors. Semin Roentgenol. 2005; 40:90–97.7. Finberg KE, Sequist LV, Joshi VA, Muzikansky A, Miller JM, Han M, et al. Mucinous differentiation correlates with absence of EGFR mutation and presence of KRAS mutation in lung adenocarcinomas with bronchioloalveolar features. J Mol Diagn. 2007; 9:320–326.8. Ioachimescu OC, Mehta AC. From cystic pulmonary airway malformation, to bronchioloalveolar carcinoma and adenocarcinoma of the lung. Eur Respir J. 2005; 26:1181–1187.9. Berger KL, Nicholson SA, Dehdashti F, Siegel BA. FDG PET evaluation of mucinous neoplasms: correlation of FDG uptake with histopathologic features. AJR Am J Roentgenol. 2000; 174:1005–1008.10. Cook GJ, Wegner EA, Fogelman I. Pitfalls and artifacts in 18FDG PET and PET/CT oncologic imaging. Semin Nucl Med. 2004; 34:122–133.