Restor Dent Endod.
2012 Mar;37(1):61-65. 10.5395/rde.2012.37.1.61.
Pulp necrosis following luxated injury to teeth in a patient with uncontrolled type II diabetes mellitus: a case report
- Affiliations
-
- 1Department of Conservative Dentistry, Yonsei University College of Dentistry, Seoul, Korea. chanyoungl@yuhs.ac
- KMID: 1995686
- DOI: http://doi.org/10.5395/rde.2012.37.1.61
Abstract
- Patients with diabetes mellitus show delayed wound healing and increased susceptibility to infection. Therefore, the effects of diabetes on pulpal and periodontal healing should be taken into consideration when treating diabetic dental traumatized patients. This case presents the treatment for dental traumatized 20 yr old female with uncontrolled type II diabetes. The traumatized upper central incisors had showed pulpal healing in early days. However, 7 mon after the trauma, the teeth had been diagnosed with pulp necrosis with apical abscess. Eventually, non surgical root canal treatment on the teeth had been performed.
MeSH Terms
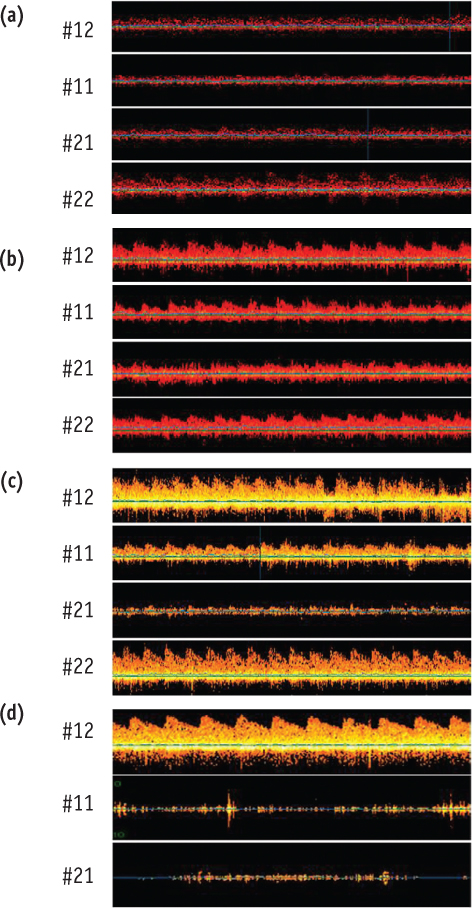
Figure
Reference
-
1. Andreasen FM, Pedersen BV. Prognosis of luxated permanent teeth-the development of pulp necrosis. Endod Dent Traumatol. 1985. 1:207–220.2. Roy S, Trudeau K, Roy S, Behl Y, Dhar S, Chronopoulos A. New insights into hyperglycemia-induced molecular changes in microvascular cells. J Dent Res. 2010. 89:116–127.
Article3. Delamaire M, Maugendre D, Moreno M, Le Goff MC, Allannic H, Genetet B. Impaired leucocyte functions in diabetic patients. Diabet Med. 1997. 14:29–34.
Article4. McMahon MM, Bistrian BR. Host defenses and susceptibility to infection in patients with diabetes mellitus. Infect Dis Clin North Am. 1995. 9:1–9.
Article5. Andreasen FM. Transient apical breakdown and its relation to color and sensibility changes after luxation injuries to teeth. Endod Dent Traumatol. 1986. 2:9–19.
Article6. Andreasen FM. Transient root resorption after dental trauma: the clinician's dilemma. J Esthet Restor Dent. 2003. 15:80–92.
Article7. Andreasen FM. Histological and bacteriological study of pulps extirpated after luxation injuries. Endod Dent Traumatol. 1988. 4:170–181.
Article8. Evans D, Reid J, Strang R, Stirrups D. A comparison of laser Doppler flowmetry with other methods of assessing the vitality of traumatised anterior teeth. Endod Dent Traumatol. 1999. 15:284–290.
Article9. Lee JY, Yanpiset K, Sigurdsson A, Vann WF Jr. Laser Doppler flowmetry for monitoring traumatized teeth. Dent Traumatol. 2001. 17:231–235.
Article10. Mesaros SV, Trope M. Revascularization of traumatized teeth assessed by laser Doppler flowmetry: case report. Endod Dent Traumatol. 1997. 13:24–30.
Article11. Yoon MJ, Kim E, Lee SJ, Bae YM, Kim S, Park SH. Pulpal blood flow measurement with ultrasound Doppler imaging. J Endod. 2010. 36:419–422.
Article12. Yoon TS, Kong HG, Kim E. Pulp vitality and coronal discoloration following traumatic injuries. J Korean Acad Conserv Dent. 2010. 35:492–496.
Article13. Kim JH, Bae KS, Seo DG, Hong ST, Lee Y, Hong SP, Kum KY. The role of type 2 diabetes as a predisposing risk factor on the pulpo-periapical pathogenesis: review article. J Korean Acad Conserv Dent. 2009. 34:169–176.
Article14. He H, Liu R, Desta T, Leone C, Gerstenfeld LC, Graves DT. Diabetes causes decreased osteoclastogenesis, reduced bone formation, and enhanced apoptosis of osteoblastic cells in bacteria stimulated bone loss. Endocrinology. 2004. 145:447–452.
Article15. Britto LR, Katz J, Guelmann M, Heft M. Periradicular radiographic assessment in diabetic and control individuals. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003. 96:449–452.
Article16. Fouad AF, Burleson J. The effect of diabetes mellitus on endodontic treatment outcome: data from an electronic patient record. J Am Dent Assoc. 2003. 134:43–51.17. Wang CH, Chueh LH, Chen SC, Feng YC, Hsiao CK, Chiang CP. Impact of diabetes mellitus, hypertension, and coronary artery disease on tooth extraction after nonsurgical endodontic treatment. J Endod. 2011. 37:1–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect On Endodontic Drainage Of The Luxated Tooth In Reduction And Fixation Of Compound Alveolar Bone Fracture
- Antepartum Pituitary Necrosis Occurring In Pregnancy with Uncontrolled Gestational Diabetes Mellitus: A Case Report
- Clinical Analysis of Diabetic Retinopathy According to the Type of Diabetes Mellitus
- Transient hemiparesis following laparoscopic cholecystectomy in a patient with uncontrolled diabetes mellitus: A case report
- The effect of advanced periodontitis on the dental pulp tissue