Restor Dent Endod.
2013 Feb;38(1):11-20. 10.5395/rde.2013.38.1.11.
The effect of clinical performance on the survival estimates of direct restorations
- Affiliations
-
- 1Department of Dentistry, Seoul National University School of Dentistry and Dental Research Institute, Seoul, Korea.
- 2Department of Conservative Dentistry, Seoul National University School of Dentistry and Dental Research Institute, Seoul, Korea. chobh@snu.ac.kr
- KMID: 1995471
- DOI: http://doi.org/10.5395/rde.2013.38.1.11
Abstract
OBJECTIVES
In most retrospective studies, the clinical performance of restorations had not been considered in survival analysis. This study investigated the effect of including the clinically unacceptable cases according to modified United States Public Health Service (USPHS) criteria into the failed data on the survival analysis of direct restorations as to the longevity and prognostic variables.
MATERIALS AND METHODS
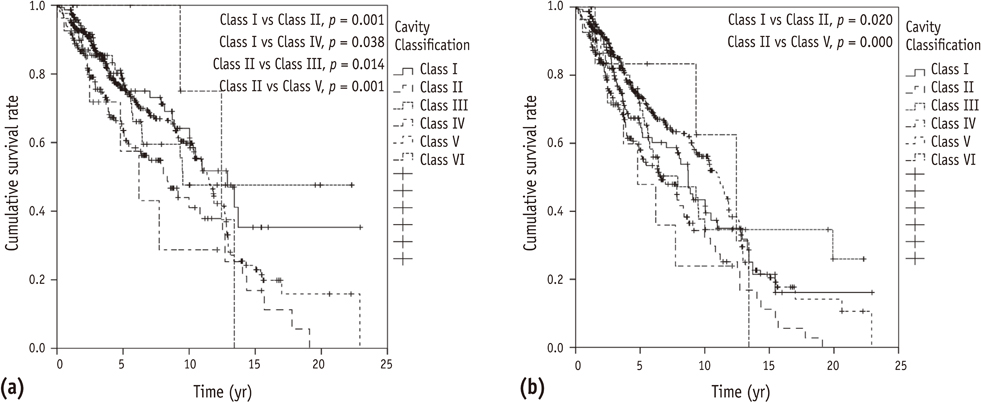
Nine hundred and sixty-seven direct restorations were evaluated. The data of 204 retreated restorations were collected from the records, and clinical performance of 763 restorations in function was evaluated according to modified USPHS criteria by two observers. The longevity and prognostic variables of the restorations were compared with a factor of involving clinically unacceptable cases into the failures using Kaplan-Meier survival analysis and Cox proportional hazard model.
RESULTS
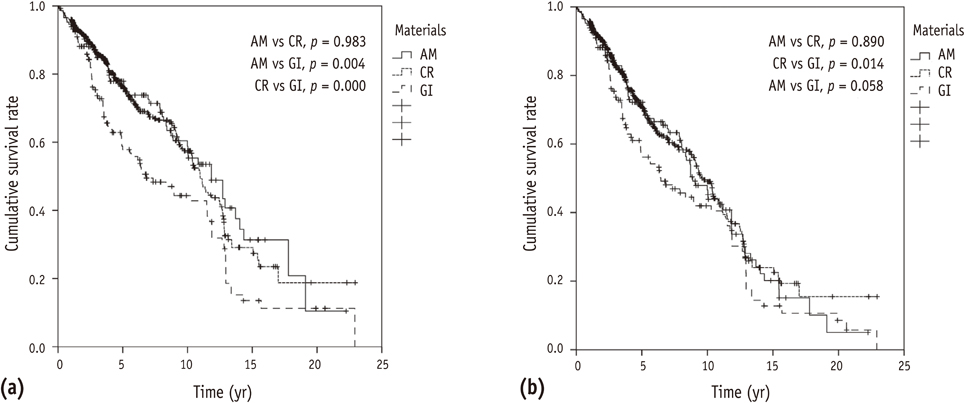
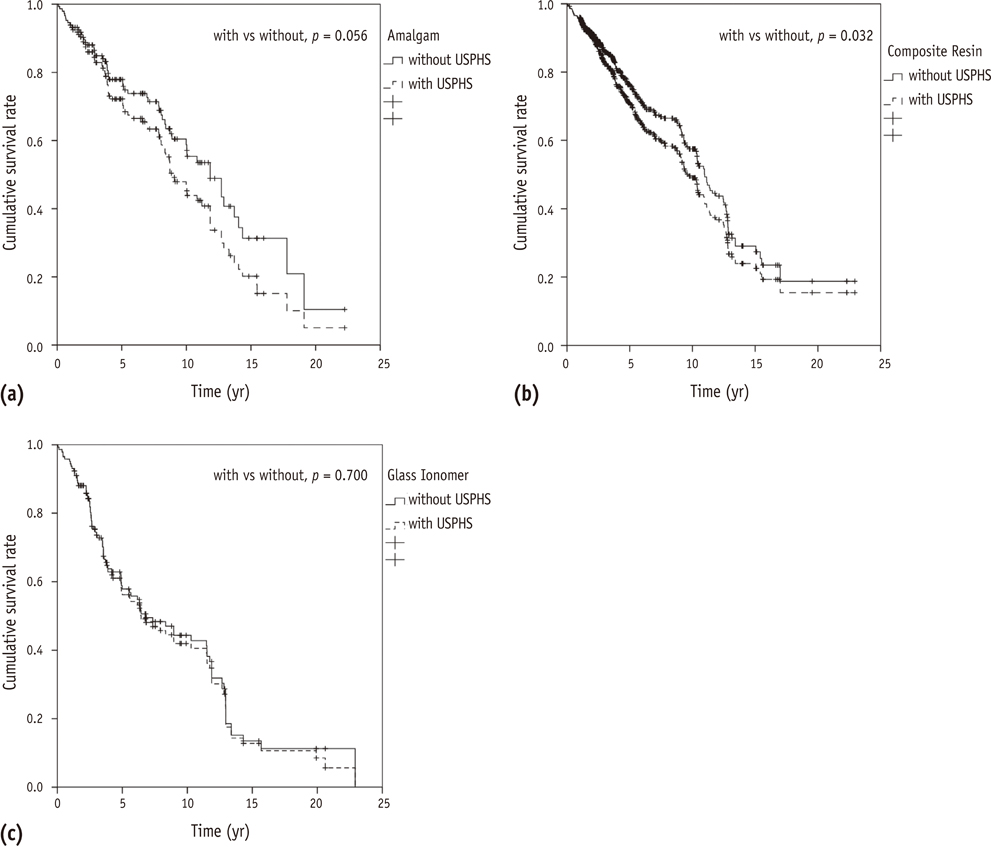
The median survival times of amalgam, composite resin and glass ionomer were 11.8, 11.0 and 6.8 years, respectively. Glass ionomer showed significantly lower longevity than composite resin and amalgam. When clinically unacceptable restorations were included into the failure, the median survival times of them decreased to 8.9, 9.7 and 6.4 years, respectively.
CONCLUSIONS
After considering the clinical performance, composite resin was the only material that showed a difference in the longevity (p < 0.05) and the significantly higher relative risk of student group than professor group disappeared in operator groups. Even in the design of retrospective study, clinical evaluation needs to be included.
MeSH Terms
Figure
Reference
-
1. Mjör IA. Amalgam and composite resin restorations: longevity and reasons for replacement. Replacement of AM restorations. Quality evaluation of dental restorations - criteria for placement and replacement. 1989. Chicago: Quintessence Publishing Co;61–68.2. Onal B, Pamir T. The two-year clinical performance of esthetic restorative materials in noncarious cervical lesions. J Am Dent Assoc. 2005. 136:1547–1555.
Article3. Chadwick B, Treasure E, Dummer P, Dunstan F, Gilmour A, Jones R, Phillips C, Stevens J, Rees J, Richmond S. Challenges with studies investigating longevity of dental restorations-a critique of a systematic review. J Dent. 2001. 29:155–161.
Article4. Manhart J, Chen H, Hamm G, Hickel R. Buonocore Memorial Lecture. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper Dent. 2004. 29:481–508.5. Opdam NJ, Bronkhorst EM, Roeters JM, Loomans BA. A retrospective clinical study on longevity of posterior composite and amalgam restorations. Dent Mater. 2007. 23:2–8.
Article6. Kubo S, Kawasaki A, Hayashi Y. Factors associated with the longevity of resin composite restorations. Dent Mater J. 2011. 30:374–383.
Article7. Goldberg AJ, Rydinge E, Santucci EA, Racz WB. Clinical evaluation methods for posterior composite restorations. J Dent Res. 1984. 63:1387–1391.
Article8. Arhun N, Celik C, Yamanel K. Clinical evaluation of resin-based composites in posterior restorations: two-year results. Oper Dent. 2010. 35:397–404.
Article9. Daou MH, Tavernier B, Meyer JM. Clinical evaluation of four different dental restorative materials: one-year results. Schweiz Monatsschr Zahnmed. 2008. 118:290–295.10. Alves dos Santos MP, Luiz RR, Maia LC. Randomized trial of resin-based restorations in Class I and Class II beveled preparations in primary molars: 48-month results. J Dent. 2010. 38:451–459.
Article11. Scholtanus JD, Huysmans MC. Clinical failure of class-II restorations of a highly viscous glass-ionomer material over a 6-year period: a retrospective study. J Dent. 2007. 35:156–162.
Article12. Mjör IA, Shen C, Eliasson ST, Richter S. Placement and replacement of restorations in general dental practice in Iceland. Oper Dent. 2002. 27:117–123.13. Roulet JF. Longevity of glass ceramic inlays and amalgam-results up to 6 years. Clin Oral Investig. 1997. 1:40–46.14. Forss H, Widström E. From amalgam to composite: selection of restorative materials and restoration longevity in Finland. Acta Odontol Scand. 2001. 59:57–62.
Article15. Goldstein GR. The longevity of direct and indirect posterior restorations is uncertain and may be affected by a number of dentist-, patient-, and material-related factors. J Evid Based Dent Pract. 2010. 10:30–31.
Article16. Antony K, Genser D, Heibinger C, Windisch F. Longevity of dental amalgam in comparison to composite materials. GMS Health Technol Assess. 2008. 4:Doc12.17. Rho YJ, Namgung C, Jin BH, Lim BS, Cho BH. Longevity of direct restorations in stress-bearing posterior cavities: a retrospective study. Oper Dent. 2000. (in press).
Article18. Mjör IA. The reasons for replacement and the age of failed restorations in general dental practice. Acta Odontol Scand. 1997. 55:58–63.
Article19. Mjör IA, Dahl JE, Moorhead JE. Age of restorations at replacement in permanent teeth in general dental practice. Acta Odontol Scand. 2000. 58:97–101.
Article20. da Rosa Rodolpho PA, Cenci MS, Donassollo TA, Loguércio AD, Demarco FF. A clinical evaluation of posterior composite restorations: 17-year findings. J Dent. 2006. 34:427–435.
Article21. Burke FJ, Cheung SW, Mjör IA, Wilson NH. Restoration longevity and analysis of reasons for the placement and replacement of restorations provided by vocational dental practitioners and their trainers in the United Kingdom. Quintessence Int. 1999. 30:234–242.22. Bernardo M, Luis H, Martin MD, Leroux BG, Rue T, Leitão J, DeRouen TA. Survival and reasons for failure of amalgam versus composite posterior restorations placed in a randomized clinical trial. J Am Dent Assoc. 2007. 138:775–783.
Article23. Van Nieuwenhuysen JP, D'Hoore W, Carvalho J, Qvist V. Long-term evaluation of extensive restorations in permanent teeth. J Dent. 2003. 31:395–405.
Article24. Demarco FF, Corrêa MB, Cenci MS, Moraes RR, Opdam NJ. Longevity of posterior composite restorations: not only a matter of materials. Dent Mater. 2012. 28:87–101.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- 1 year follow-up study of direct and indirect composite restorations
- 5 Year Cumulative Survival Rate of Composite Resin Restorations in Permanent First Molars
- Clinical performance and failures of zirconia-based fixed partial dentures: a review literature
- Retrospective study of fracture survival in endodontically treated molars: the effect of single-unit crowns versus direct-resin composite restorations
- Long-Term Evaluation of Direct Composite Resin Restoration for Traumatic Anterior Crown Fractures in Children and Adolescents