Korean J Urol.
2012 Jan;53(1):29-33. 10.4111/kju.2012.53.1.29.
Effect of Bladder Neck Preservation and Posterior Urethral Reconstruction during Robot-Assisted Laparoscopic Radical Prostatectomy for Urinary Continence
- Affiliations
-
- 1Department of Urology, Dong-A University College of Medicine, Busan, Korea. sunggt@dau.ac.kr
- KMID: 1988820
- DOI: http://doi.org/10.4111/kju.2012.53.1.29
Abstract
- PURPOSE
To report our results on urinary continence after bladder neck preservation (BNP) and posterior urethral reconstruction (PUR) during robot-assisted laparoscopic radical prostatectomy (RALP).
MATERIALS AND METHODS
Data from 107 patients who underwent RALP were compared on the basis of whether the patients underwent BNP and PUR, BNP only, or the standard technique (ST). In group A (n=31 patients), ST was performed by using Ven velthoven continuous suturing for urethrovesical anastomosis. In group B (n=28 patients), ST with only PUR was performed. In group C (n=48 patients), both the BNP and PUR techniques were used. "Recovery of continence" was defined as the use of 1 pad (50 ml) or less within 24 hours.
RESULTS
The three groups were comparable in terms of patient demographics. The mean operative time and the mean blood loss decreased significantly from group A to group C (p=0.021 for mean operative time and p=0.004 for the mean blood loss). Mean catheterization time was 8.9, 7.8, and 7.1 days in each group (p=0.047). Early return of urinary continence at 3 months was observed in group B (89.2%) and group C (90.6%) compared with group A (71%). However, continence at 6 months was comparable in the 3 groups (87.5% in group A, 92.8% in group B, and 92.3% in group C). Rates of positive surgical margins decreased from 30.2% in group A to 20% in group B and 12% in group C.
CONCLUSIONS
BNP and PUR during RALP showed a favorable impact on the early postoperative recovery of continence while not affecting positive surgical margins.
MeSH Terms
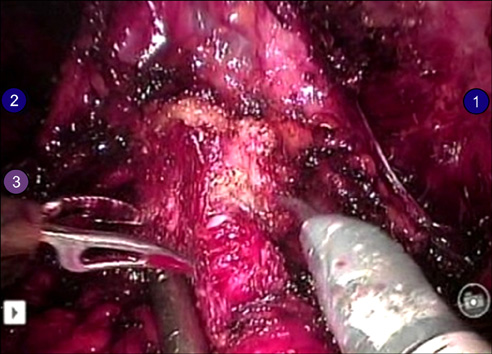
Figure
Reference
-
1. Cho JW, Kim TH, Sung GT. Laparoscopic radical prostatectomy versus robot-assisted laparoscopic radical prostatectomy: a single surgeon's experience. Korean J Urol. 2009. 50:1198–1202.2. Rassweiler J, Sentker L, Seemann O, Hatzinger M, Rumpelt HJ. Laparoscopic radical prostatectomy with the Heilbronn technique: an analysis of the first 180 cases. J Urol. 2001. 166:2101–2108.3. Eden CG, Cahill D, Vass JA, Adams TH, Dauleh MI. Laparoscopic radical prostatectomy: the initial UK series. BJU Int. 2002. 90:876–882.4. Guillonneau B, el-Fettouh H, Baumert H, Cathelineau X, Doublet JD, Fromont G, et al. Laparoscopic radical prostatectomy: oncological evaluation after 1,000 cases a Montsouris Institute. J Urol. 2003. 169:1261–1266.5. Salomon L, Anastasiadis AG, Katz R, De La Taille A, Saint F, Vordos D, et al. Urinary continence and erectile function: a prospective evaluation of functional results after radical laparoscopic prostatectomy. Eur Urol. 2002. 42:338–343.6. Peyromaure M, Ravery V, Boccon-Gibod L. The management of stress urinary incontinence after radical prostatectomy. BJU Int. 2002. 90:155–161.7. Burnett AL, Mostwin JL. In situ anatomical study of the male urethral sphincteric complex: relevance to continence preservation following major pelvic surgery. J Urol. 1998. 160:1301–1306.8. Rocco F, Carmignani L, Acquati P, Gadda F, Dell'Orto P, Rocco B, et al. Restoration of posterior aspect of rhabdosphincter shortens continence time after radical retropubic prostatectomy. J Urol. 2006. 175:2201–2206.9. Rocco B, Gregori A, Stener S, Santoro L, Bozzola A, Galli S, et al. Posterior reconstruction of the rhabdosphincter allows a rapid recovery of continence after transperitoneal videolaparoscopic radical prostatectomy. Eur Urol. 2007. 51:996–1003.10. Duthie JB, Pickford JE, Gilling PJ. Robot-assisted laparoscopic prostatectomy: a 2010 update. N Z Med J. 2010. 123:30–34.11. Rebuck DA, Haywood S, McDermott K, Perry KT, Nadler RB. What is the long-term relevance of clinically detected postoperative anastomotic urine leakage after robotic-assisted laparoscopic prostatectomy. BJU Int. 2011. 108:733–738.12. Asimakopoulos AD, Annino F, D'Orazio A, Pereira CF, Mugnier C, Hoepffner JL, et al. Complete periprostatic anatomy preservation during robot-assisted laparoscopic radical prostatectomy (RALP): the new pubovesical complex-sparing technique. Eur Urol. 2010. 58:407–417.13. Jeong W, Araki M, Park SY, Lee YH, Kumon H, Hong SJ, Rha KH. Robot-assisted laparoscopic radical prostatectomy in the Asian population: modified port configuration and ultradissection. Int J Urol. 2010. 17:297–300.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effectiveness of Cystography-Measured Bladder Neck Elevation at Predicting the Return of Continence After Robot-Assisted Radical Prostatectomy
- Effect of Posterior Urethral Reconstruction (PUR) in Early Recovery of Urinary Continence after Robotic-Assisted Radical Prostatectomy
- Floating Hem-o-Lok Clips in the Bladder without Stone Formation after Robot-Assisted Laparoscopic Radical Prostatectomy
- Erratum: Robot-Assisted Laparoscopic Radical Prostatectomy
- Impact of Posterior Urethral Plate Repair on Continence Following Robot-Assisted Laparoscopic Radical Prostatectomy