Korean J Urol.
2014 Mar;55(3):219-221. 10.4111/kju.2014.55.3.219.
Schwannoma of the Scrotum: Case Report and Review of the Literature
- Affiliations
-
- 1Department of Pathology, Jawaharlal Nehru Medical College, Aligarh Muslim University, Aligarh, India. shahidaftab@gmail.com
- 2Department of Radiodiagnosis, Jawaharlal Nehru Medical College, Aligarh Muslim University, Aligarh, India.
- KMID: 1988428
- DOI: http://doi.org/10.4111/kju.2014.55.3.219
Abstract
- Schwannomas are benign nerve sheath tumors composed of Schwann cells, which normally produce the insulating myelin sheath covering the peripheral nerves. Common locations include the head, neck, mediastinum, and retroperitoneum. These tumors are usually asymptomatic until they become large and compress the surrounding tissues. Most schwannomas occur during the third and fourth decades of life, with an equal gender distribution. We present the case of a schwannoma that originated in the scrotum.
Keyword
MeSH Terms
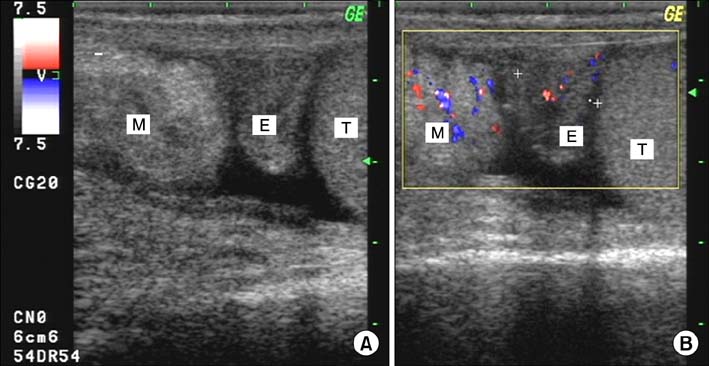
Figure
Reference
-
1. Matsui F, Kobori Y, Takashima H, Amano T, Takemae K. A case of intrascrotal schwannoma. Hinyokika Kiyo. 2002; 48:749–751.2. Latchamsetty KC, Elterman L, Coogan CL. Schwannoma of a seminal vesicle. Urology. 2002; 60:515.3. Zarate Rodríguez E, Fernandez Gonzalez I, Lujan Galan M, Ortega Munoz P, Berenguer Sánchez A. Schwannoma of the scrotum: report of case and review of the literature. Actas Urol Esp. 1997; 21:1012–1013.4. Safak M, Baltaci S, Ozer G, Turkolmez K, Uluoglu O. Long-term outcome of a patient with intrascrotal extratesticular malignant schwannoma. Urol Int. 1998; 60:202–204.5. Chan PT, Tripathi S, Low SE, Robinson LQ. Case report: ancient schwannoma of the scrotum. BMC Urol. 2007; 7:1.6. Rosai J, Ackerman LV. Ackerman's surgical pathology. 9th ed. New York: Mosby;2004.7. Isobe K, Shimizu T, Akahane T, Kato H. Imaging of ancient schwannoma. AJR Am J Roentgenol. 2004; 183:331–336.8. Daneshmand S, Youssefzadeh D, Chamie K, Boswell W, Wu N, Stein JP, et al. Benign retroperitoneal schwannoma: a case series and review of the literature. Urology. 2003; 62:993–997.9. Chu YC, Yoon YH, Han HS, Han JY, Kim JM, Park IS. Malignant transformation of intrathoracic ancient neurilemmoma in a patient without von Recklinghausen's disease. J Korean Med Sci. 2003; 18:295–298.10. Jiang R, Chen JH, Chen M, Li QM. Male genital schwannoma, review of 5 cases. Asian J Androl. 2003; 5:251–254.