J Cardiovasc Ultrasound.
2014 Dec;22(4):182-188. 10.4250/jcu.2014.22.4.182.
Segmental Analysis of Right Ventricular Longitudinal Deformation in Children before and after Percutaneous Closure of Atrial Septal Defect
- Affiliations
-
- 1Department of Pediatrics, Ajou University School of Medicine, Suwon, Korea.
- 2Division of Pediatric Cardiology, College of Medicine, University of Ulsan, Seoul, Korea. pediatrist@medimail.co.kr
- KMID: 1980421
- DOI: http://doi.org/10.4250/jcu.2014.22.4.182
Abstract
- BACKGROUND
The aim of study is to identify the dependence of right ventricular (RV) free wall longitudinal deformation on ventricular loading through segmental approach in relatively large number of patients with atrial septal defect (ASD).
METHODS
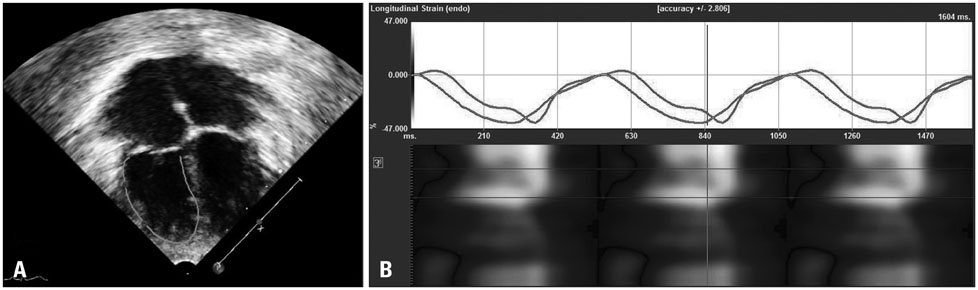
Patients with ASD (n = 114) and age matched healthy children (n = 60) were echocardiographically examined the day before percutaneous device closure and within 24 hours afterwards. RV free wall deformation parameters, strain (small je, Ukrainian) and strain rate (SR), were analyzed in the apical (small je, Ukrainian(A), SR(A)) and basal (small je, Ukrainian(B), SR(B)) segments. Measured deformation parameters were adjusted for RV size (small je, Ukrainian(AL), SR(AL), small je, Ukrainian(BL), SR(BL)) by multiplying by body surface area indexed RV longitudinal dimension. Regression analyses determined the relationships of these deformation parameters with RV loading parameters that were measured by catheterization.
RESULTS
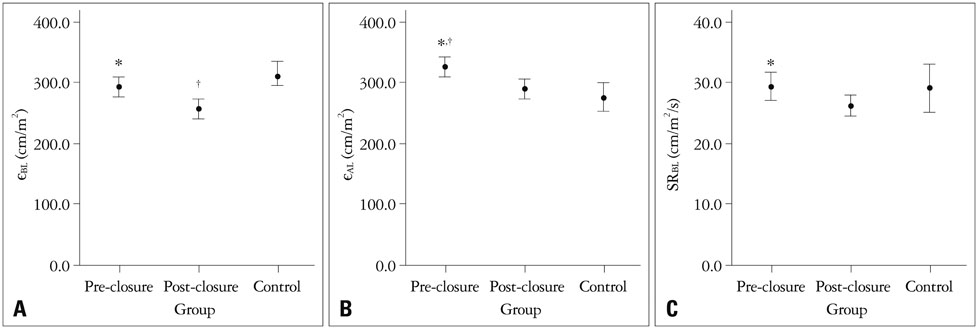
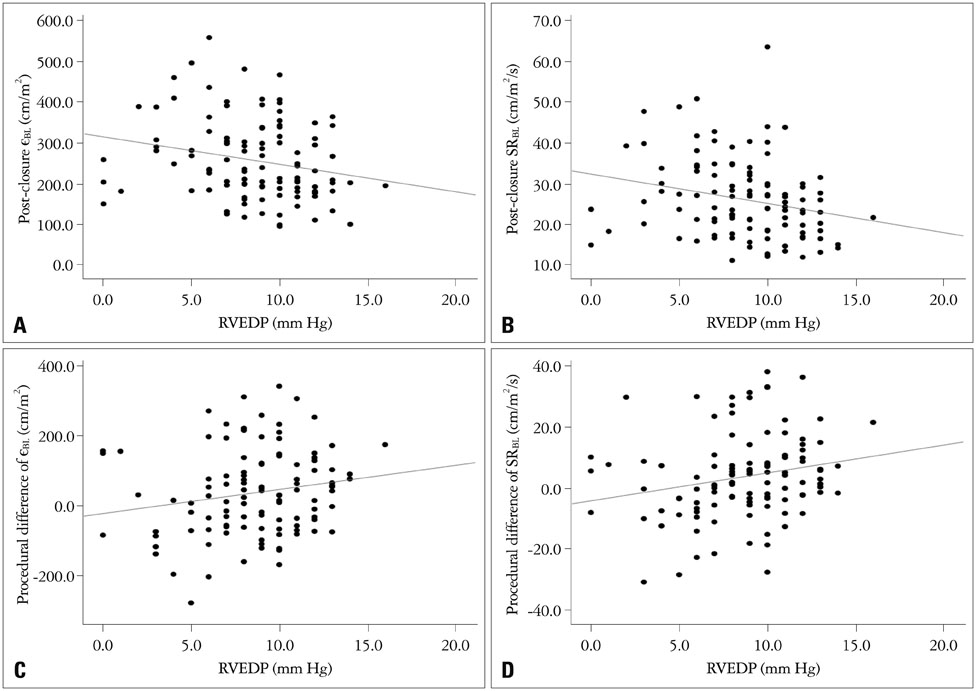
small je, Ukrainian(BL) and SR(BL) were not different between pre-closure patients and controls (p = 0.245, p = 0.866), and were decreased post-closure (p = 0.001, p = 0.018). Post-closure small je, Ukrainian(BL) was lower than in controls (p = 0.001). Pre-closure small je, Ukrainian(AL) and SR(AL) were higher than in controls (p = 0.001, p < 0.001), but decreased after closure (all p < 0.001). The pulmonary to systemic flow ratio was related to procedural differences of small je, Ukrainian(BL) (p = 0.017) and of SR(BL) (p = 0.019). RV end diastolic pressure was negatively related to post-closure small je, Ukrainian(BL) (p = 0.020) and post-closure SR(BL) (p = 0.012), and the procedural SR(BL) difference (p = 0.027).
CONCLUSION
The longitudinal deformation of the RV basal segment is dependent and its remodeling is also dependent on volume loading in children with ASD.
MeSH Terms
Figure
Cited by 1 articles
-
Geometric and Functional Change of Both Ventricles after Atrial Ventricular Septal Defect Closure
Soo-Jin Kim
J Cardiovasc Ultrasound. 2014;22(4):180-181. doi: 10.4250/jcu.2014.22.4.180.
Reference
-
1. Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002; 39:1890–1900.
Article2. Jeong JA, Kim YM, Lee HS, Kwon TC, Kang CM. Statistical study on congenital heart disease. Korean Circ J. 1989; 19:89–96.
Article3. Hoffman JI, Christianson R. Congenital heart disease in a cohort of 19,502 births with long-term follow-up. Am J Cardiol. 1978; 42:641–647.
Article4. Craig RJ, Selzer A. Natural history and prognosis of atrial septal defect. Circulation. 1968; 37:805–815.
Article5. Attie F, Rosas M, Granados N, Zabal C, Buendía A, Calderón J. Surgical treatment for secundum atrial septal defects in patients >40 years old. A randomized clinical trial. J Am Coll Cardiol. 2001; 38:2035–2042.
Article6. Konstantinides S, Geibel A, Olschewski M, Görnandt L, Roskamm H, Spillner G, Just H, Kasper W. A comparison of surgical and medical therapy for atrial septal defect in adults. N Engl J Med. 1995; 333:469–473.
Article7. D'hooge J, Heimdal A, Jamal F, Kukulski T, Bijnens B, Rademakers F, Hatle L, Suetens P, Sutherland GR. Regional strain and strain rate measurements by cardiac ultrasound: principles, implementation and limitations. Eur J Echocardiogr. 2000; 1:154–170.8. Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010; 23:685–713. quiz 786-8.
Article9. Missant C, Rex S, Claus P, Mertens L, Wouters PF. Load-sensitivity of regional tissue deformation in the right ventricle: isovolumic versus ejection-phase indices of contractility. Heart. 2008; 94:e15.
Article10. Dambrauskaite V, Delcroix M, Claus P, Herbots L, D'hooge J, Bijnens B, Rademakers F, Sutherland GR. Regional right ventricular dysfunction in chronic pulmonary hypertension. J Am Soc Echocardiogr. 2007; 20:1172–1180.
Article11. Sutherland GR, Di Salvo G, Claus P, D'hooge J, Bijnens B. Strain and strain rate imaging: a new clinical approach to quantifying regional myocardial function. J Am Soc Echocardiogr. 2004; 17:788–802.
Article12. Kjaergaard J, Sogaard P, Hassager C. Right ventricular strain in pulmonary embolism by Doppler tissue echocardiography. J Am Soc Echocardiogr. 2004; 17:1210–1212.
Article13. Chow PC, Liang XC, Cheung EW, Lam WW, Cheung YF. New two-dimensional global longitudinal strain and strain rate imaging for assessment of systemic right ventricular function. Heart. 2008; 94:855–859.
Article14. Eyskens B, Ganame J, Claus P, Boshoff D, Gewillig M, Mertens L. Ultrasonic strain rate and strain imaging of the right ventricle in children before and after percutaneous closure of an atrial septal defect. J Am Soc Echocardiogr. 2006; 19:994–1000.
Article15. Abd El, Hui W, Timme J, Ewert P, Berger F, Dsebissowa F, Hetzer R, Lange PE, Abdul-Khaliq H. Analysis of atrial and ventricular performance by tissue Doppler imaging in patients with atrial septal defects before and after surgical and catheter closure. Echocardiography. 2005; 22:579–585.
Article16. Van De Bruaene A, Buys R, Vanhees L, Delcroix M, Voigt JU, Budts W. Regional right ventricular deformation in patients with open and closed atrial septal defect. Eur J Echocardiogr. 2011; 12:206–213.
Article17. Dragulescu A, Grosse-Wortmann L, Redington A, Friedberg MK, Mertens L. Differential effect of right ventricular dilatation on myocardial deformation in patients with atrial septal defects and patients after tetralogy of Fallot repair. Int J Cardiol. 2013; 168:803–810.
Article18. Bussadori C, Oliveira P, Arcidiacono C, Saracino A, Nicolosi E, Negura D, Piazza L, Micheletti A, Chessa M, Butera G, Dua JS, Carminati M. Right and left ventricular strain and strain rate in young adults before and after percutaneous atrial septal defect closure. Echocardiography. 2011; 28:730–737.
Article19. Di Salvo G, Drago M, Pacileo G, Carrozza M, Santoro G, Bigazzi MC, Caso P, Russo MG, Carminati M, Calabró R. Comparison of strain rate imaging for quantitative evaluation of regional left and right ventricular function after surgical versus percutaneous closure of atrial septal defect. Am J Cardiol. 2005; 96:299–302.
Article20. Jategaonkar SR, Scholtz W, Butz T, Bogunovic N, Faber L, Horstkotte D. Two-dimensional strain and strain rate imaging of the right ventricle in adult patients before and after percutaneous closure of atrial septal defects. Eur J Echocardiogr. 2009; 10:499–502.
Article21. Haycock GB, Schwartz GJ, Wisotsky DH. Geometric method for measuring body surface area: a height-weight formula validated in infants, children, and adults. J Pediatr. 1978; 93:62–66.
Article22. Galderisi M, Benjamin EJ, Evans JC, D'Agostino RB, Fuller DL, Lehman B, Wolf PA, Levy D. Intra- and interobserver reproducibility of Doppler-assessed indexes of left ventricular diastolic function in a population-based study (the Framingham Heart Study). Am J Cardiol. 1992; 70:1341–1346.
Article23. Marciniak A, Claus P, Sutherland GR, Marciniak M, Karu T, Baltabaeva A, Merli E, Bijnens B, Jahangiri M. Changes in systolic left ventricular function in isolated mitral regurgitation. A strain rate imaging study. Eur Heart J. 2007; 28:2627–2636.
Article24. Naito H, Arisawa J, Harada K, Yamagami H, Kozuka T, Tamura S. Assessment of right ventricular regional contraction and comparison with the left ventricle in normal humans: a cine magnetic resonance study with presaturation myocardial tagging. Br Heart J. 1995; 74:186–191.
Article25. Teske AJ, Prakken NH, De Boeck BW, Velthuis BK, Martens EP, Doevendans PA, Cramer MJ. Echocardiographic tissue deformation imaging of right ventricular systolic function in endurance athletes. Eur Heart J. 2009; 30:969–977.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Extraction of an Embolized Atrial Septal Defect Occluder Device into Pulmonary Artery after Percutaneous Closure
- Subacute, Silent Embolization of Amplatzer Atrial Septal Defect Closure Device to the Pulmonary Artery
- Echocardiographic Evaluation of Atrial Septal Defect Device Closure
- Emergent Surgical Intervention for Embolization of Atrial Septal Defect Closure Device
- Comparison of Efficacy of Transcatheter Closure of Atrial Septal Defect with Amplatzer Septal Occluder between Children and Adult