J Korean Assoc Oral Maxillofac Surg.
2013 Dec;39(6):257-262. 10.5125/jkaoms.2013.39.6.257.
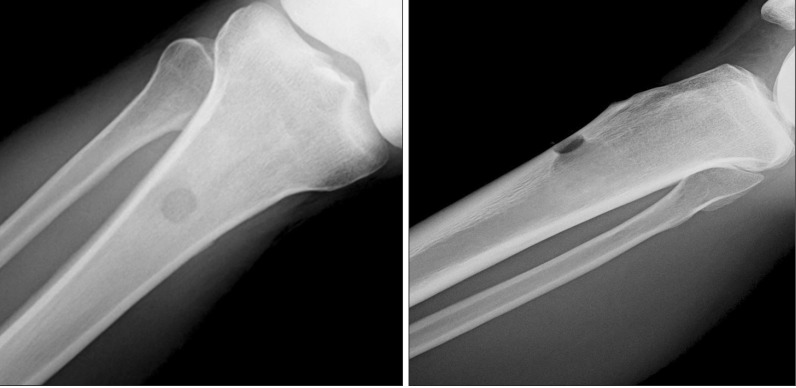
Tibial bone fractures occurring after medioproximal tibial bone grafts for oral and maxillofacial reconstruction
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Department of Dentistry, Inha University School of Medicine, Incheon, Korea. kik@inha.ac.kr
- KMID: 1960974
- DOI: http://doi.org/10.5125/jkaoms.2013.39.6.257
Abstract
OBJECTIVES
Oral and maxillofacial defects often require bone grafts to restore missing tissues. Well-recognized donor sites include the anterior and posterior iliac crest, rib, and intercalvarial diploic bone. The proximal tibia has also been explored as an alternative donor site. The use of the tibia for bone graft has many benefits, such as procedural ease, adequate volume of cancellous and cortical bone, and minimal complications. Although patients rarely complain of pain, swelling, discomfort, or dysfunction, such as gait disturbance, both patients and surgeons should pay close attention to such after effects due to the possibility of tibial fracture. The purpose of this study is to analyze tibial fractures that occurring after osteotomy for a medioproximal tibial graft.
MATERIALS AND METHODS
An analysis was intended for patients who underwent medioproximal tibial graft between March 2004 and December 2011 in Inha University Hospital. A total of 105 subjects, 30 females and 75 males, ranged in age from 17 to 78 years. We investigated the age, weight, circumstance, and graft timing in relation to tibial fracture.
RESULTS
Tibial fractures occurred in four of 105 patients. There were no significant differences in graft region, shape, or scale between the fractured and non-fractured patients.
CONCLUSION
Patients who undergo tibial grafts must be careful of excessive external force after the operation.
Keyword
MeSH Terms
Figure
Reference
-
1. Lee CY. An in-office technique for harvesting tibial bone: outcomes in 8 patients. J Oral Implantol. 2003; 29:181–184. PMID: 12964798.2. Jakse N, Seibert FJ, Lorenzoni M, Eskici A, Pertl C. A modified technique of harvesting tibial cancellous bone and its use for sinus grafting. Clin Oral Implants Res. 2001; 12:488–494. PMID: 11564109.
Article3. Herford AS, King BJ, Audia F, Becktor J. Medial approach for tibial bone graft: anatomic study and clinical technique. J Oral Maxillofac Surg. 2003; 61:358–363. PMID: 12618977.
Article4. Catone GA, Reimer BL, McNeir D, Ray R. Tibial autogenous cancellous bone as an alternative donor site in maxillofacial surgery: a preliminary report. J Oral Maxillofac Surg. 1992; 50:1258–1263. PMID: 1333008.
Article5. Hernández-Alfaro F, Martí C, Biosca MJ, Gimeno J. Minimally invasive tibial bone harvesting under intravenous sedation. J Oral Maxillofac Surg. 2005; 63:464–470. PMID: 15789317.
Article6. Baek MK, Kim IK, Cho HY, Chang KS, Park SH, Park JW, et al. A retrospective analysis of the medioproximal tibial bone graft for oral and maxillofacial reconstruction. J Korean Assoc Maxillofac Plast Reconstr Surg. 2008; 30:241–248.7. O'Keeffe RM Jr, Riemer BL, Butterfield SL. Harvesting of autogenous cancellous bone graft from the proximal tibial metaphysis. A review of 230 cases. J Orthop Trauma. 1991; 5:469–474. PMID: 1762010.8. van Damme PA, Merkx MA. A modification of the tibial bone-graft-harvesting technique. Int J Oral Maxillofac Surg. 1996; 25:346–348. PMID: 8961013.
Article9. van Damme PA, Merkx MA. Fracture of the tibia after the modified tibial bone-graft-harvesting technique: a report of two cases. J Craniomaxillofac Surg. 1998; 26(Suppl 1):197. PMID: 9777498.10. Besly W, Ward Booth P. Technique for harvesting tibial cancellous bone modified for use in children. Br J Oral Maxillofac Surg. 1999; 37:129–133. PMID: 10371319.
Article11. Lezcano FJ, Cagigal BP, Cantera JM, de la Peña Varela G, Blanco RF, Hernández AV. Technical note: medial approach for proximal tibia bone graft using a manual trephine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 104:e11–e17. PMID: 17482845.12. Marchena JM, Block MS, Stover JD. Tibial bone harvesting under intravenous sedation: morbidity and patient experiences. J Oral Maxillofac Surg. 2002; 60:1151–1154. PMID: 12378490.
Article13. Hughes CW, Revington PJ. The proximal tibia donor site in cleft alveolar bone grafting: experience of 75 consecutive cases. J Craniomaxillofac Surg. 2002; 30:12–16. PMID: 12064877.
Article14. Thor A, Farzad P, Larsson S. Fracture of the tibia: complication of bone grafting to the anterior maxilla. Br J Oral Maxillofac Surg. 2006; 44:46–48. PMID: 15907349.
Article15. Alt V, Meeder PJ, Seligson D, Schad A, Atienza C Jr. The proximal tibia metaphysis: a reliable donor site for bone grafting? Clin Orthop Relat Res. 2003; (414):315–321. PMID: 12966306.
Article16. Vittayakittipong P, Nurit W, Kirirat P. Proximal tibial bone graft: the volume of cancellous bone, and strength of decancellated tibias by the medial approach. Int J Oral Maxillofac Surg. 2012; 41:531–536. PMID: 22133867.
Article17. Gerressen M, Riediger D, Marx R, Saxe J, Ghassemi A. Stability behavior of human tibias after bone removal--comparative examination in 15 cadaver tibia pairs. J Oral Maxillofac Surg. 2010; 68:60–67. PMID: 20006156.
Article18. Morrison JB. The mechanics of the knee joint in relation to normal walking. J Biomech. 1970; 3:51–61. PMID: 5521530.
Article19. Nisell R. Mechanics of the knee. A study of joint and muscle load with clinical applications. Acta Orthop Scand Suppl. 1985; 216:1–42. PMID: 3865491.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A retrospective analysis of the medioproximal tibial bone graft for oral and maxillofacial reconstruction
- A clinical comparative study between anterior iliac and proximal tibial metaphysis particulated cancellous bone grafts
- Clinical Study on Tibial Bone Graft
- Tibial Tunnel enlargement Following Arthroscopic ACL Reconstruction
- Reconstruction of alveolar clefts with iliac cancellous particulate or block bone grafts: a comparative study