J Korean Soc Spine Surg.
2005 Sep;12(3):184-191. 10.4184/jkss.2005.12.3.184.
The Influence of the Degree of Lumbar Disc Degeneration on MRI and the Amount of Removed Disc on Clinical Outcomes
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, Dong-A University, Busan, Korea. tynitus@dau.ac.kr
- KMID: 1941683
- DOI: http://doi.org/10.4184/jkss.2005.12.3.184
Abstract
- STUDY DESIGN: The influence of lumbar disc degeneration, the space-occupying ratio on MRI and the amount of removed disc on the clinical outcomes of an open discectomy were analyzed retrospectively.
OBJECTIVES
This study analyzed the pre and post-operative factors associated with the clinical outcome of an open discectomy. SUMMARY OF LITERATURE REVIEW: Much controversy still exists regarding the factors that influence the clinical outcome following an open discectomy.
MATERIALS AND METHODS
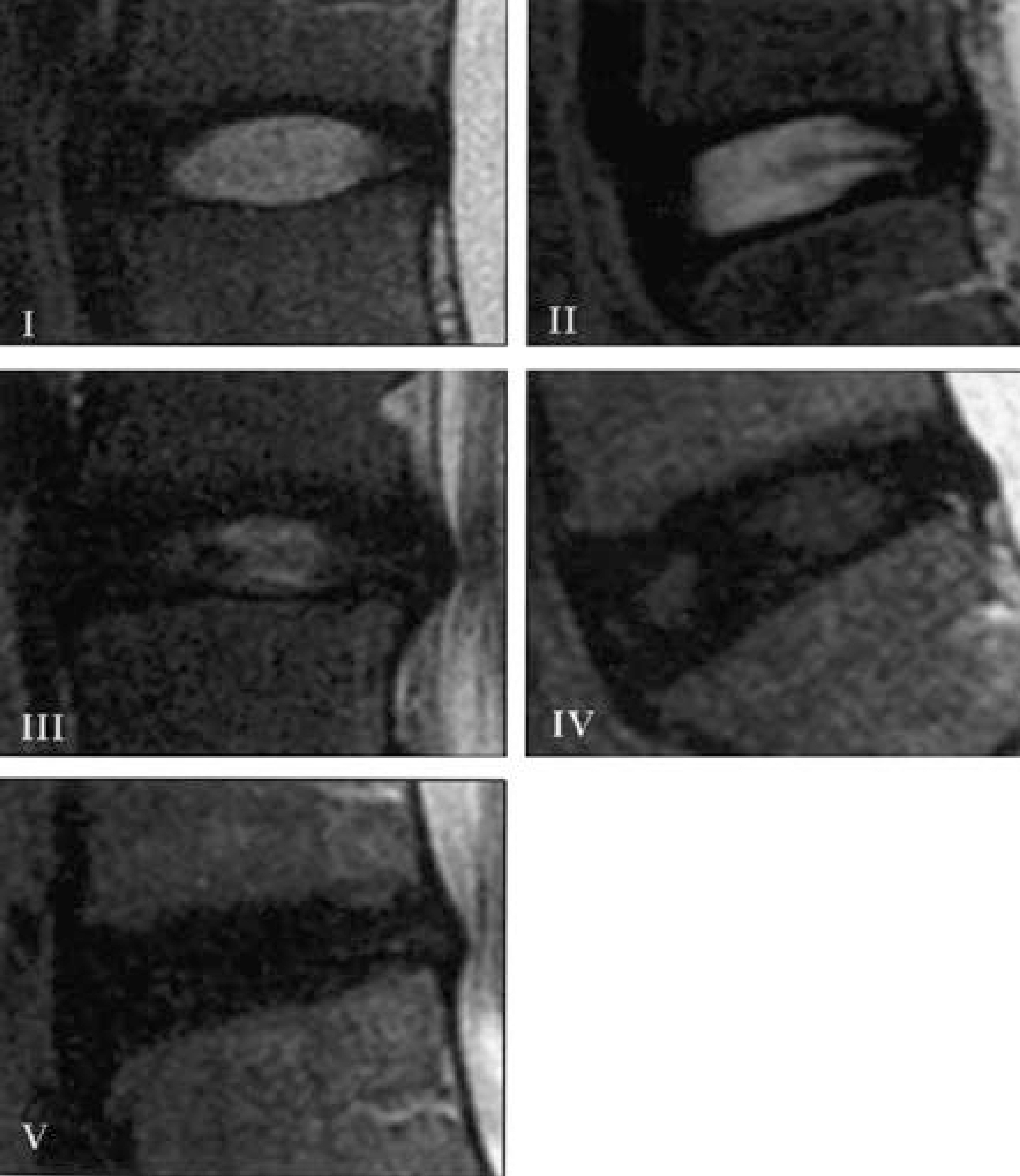
Out of 207 patients who had been treated with an open discectomy for a lumber disc herniation, between April 1997 and December 2003, 161 patients who underwent MRI with the same apparatus, with at least 6 months of follow-up, were analyzed. The study group was composed of 111 men and 50 women, with a mean age at the time of surgery of 33.1 years old. The mean follow-up period was 42 months. The degree of disc degeneration was classified according to the Thompson's classification, and the extent of the discectomy was measured by the volume. The postoperative outcomes were judged using Nayer's classification.
RESULTS
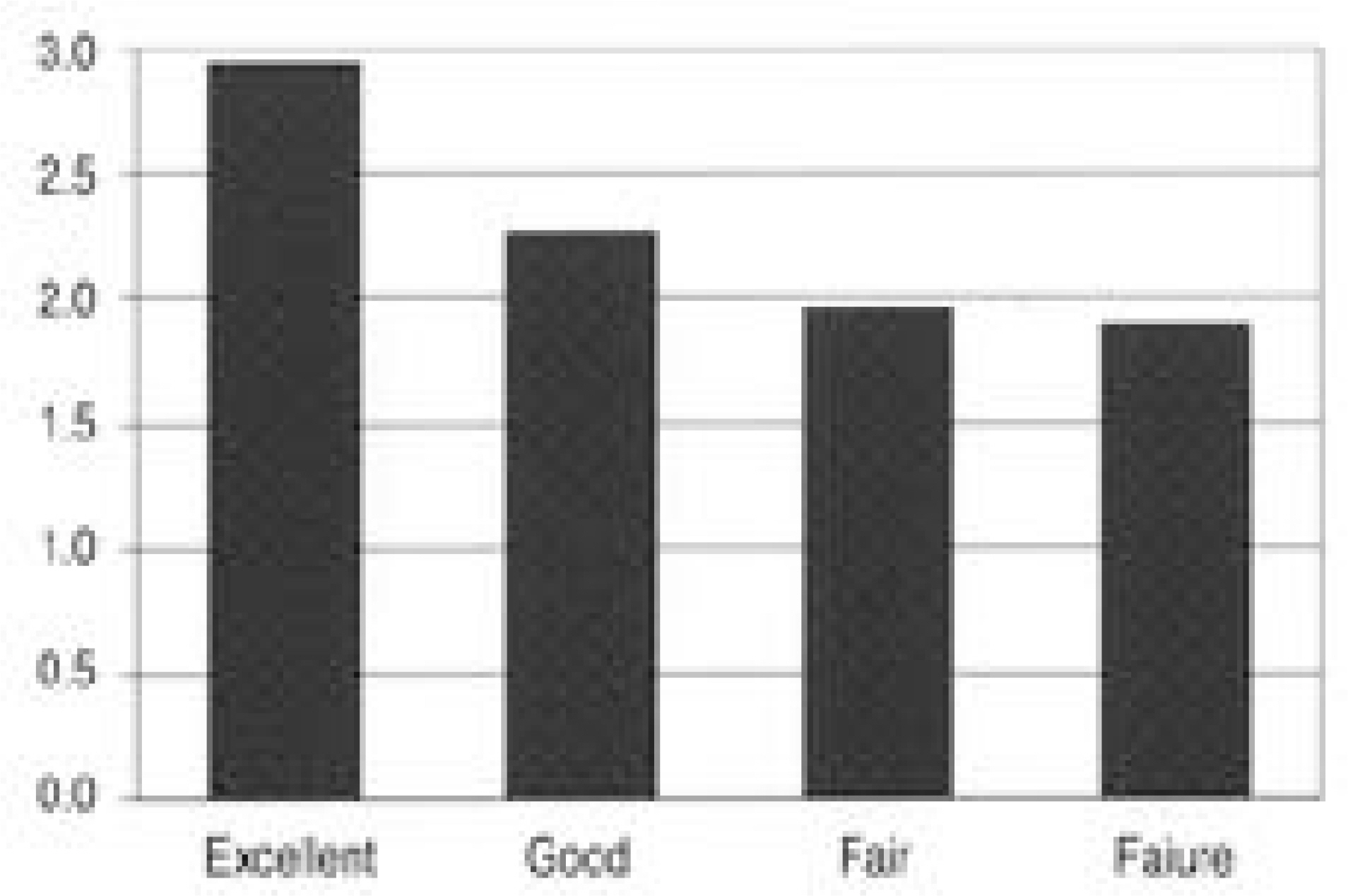
The highest frequency of disc herniation occurred at the L4-5 level, with being of the subligamentous extrusion type. The disc degeneration observed on MRI had a high statistical correlation with age (p<0.001); however, there was no statistical relationship with the level of disc herniation, sex and the amount of disc removed by discectomy (p>0.05). Clinically, 123 cases were more than fair, and 4 cases underwent reoperation due to recurrence. The clinical outcome, sex, age and space-occupying ratio were of little statistical value (p>0.05). Statistically, the greater the amount of disc removed, the better the clinical outcome (p<0.05). Those with disc degeneration classified as grade 3 from the MRI had unsatisfactory clinical outcomes (p<0.05).
CONCLUSIONS
Those with disc degeneration classified as grade 3 from the MRI had unsatisfactory clinical outcomes. The greater the amount of disc removed the more satisfactory the clinical outcomes. No statistical relationships were found between the space-occupying ratio and the clinical outcome.
MeSH Terms
Figure
Cited by 1 articles
-
Radiological and Clinical Outcome after Simple Discectomy of Central Massive Lumbar Disc Herniation
Young Do Koh, Seung Jun Rhee, Dong Jun Kim
J Korean Soc Spine Surg. 2010;17(4):169-176. doi: 10.4184/JKSS.2010.17.4.169.
Reference
-
1). Andersoon GB, Svensson H, Olden A. The intensity of work recovery in low back pain. Spine. 1983; 8:880–884.
Article2). Biering-Sorensen F. Physical measurements are risk indicators for low back trouble over a one-years period. Spine. 1984; 9:106–119.3). Colhorn E, McCall IW, Williams L. Provocative discog -raphy as a guide to planning operations on the spine. J Bone Joint Surg. 1988; 70B:267–271.4). Modic MT, Masaryk T, Wenstein MN. MRI of the spine. Radiolo Clin North Am. 1986; 24A:229–245.5). Modic MT, Parlicek W, Wernstein HA. MRI imaging of intervertebral disc disease, Radiology. 1984; 152:103–111.6). Thompson JP, Pearce RH, Schechter MT, Adams ME, Tsang IK, Bishop PB. Preliminary evaluation of a scheme for grading the gross morphology of the human intervertebral disc. Spine. 1990; 15:411–415.
Article7). Mastubara Y., et alSerial change on MRI in lumbar disc herniations treated conservatively. Neuroradiology. 1995; 37:378–383.8). Farfan HF. Mechanical disorders of the low back. Lea and Febiger;Philadelphia: p. 33–40. 1973.9). Nayer A. The late results of laminectomy for lumbar disc prolapse. J Bone Joint Surg. 1974; 56B:17–29.10). Finneson BE. Low back pain. 2nd Ed. Philadelphia: JB Lippincott Co;p. 320–326. 1980.11). Weber H. Lumbar disc herniation: a controlled, prospective study with ten years of observation. Spine. 1983; 8:131–140.
Article12). Weir BK. Prospective study of 100 lumbosacral discec -tomies. J Neurosurg. 1979; 50:238–239.13). Spangfort EV. The lumbar disc herniation. A comput -eraided ananlysis of 2504 operations. Acta orthop Scand. 142:1. 1972.14). Kim EH, Woo BC, Cho DY. Prognostic factors after conventional surgery of lumbar disc herniation-comparative study-Comparative between Non-compensator and Compensator. J Kor Spine Surg. 1997; 4:18–26.15). Tullberg T, Rydberg J, Lascsson J. Radiographic changes after lumbar discectomy: Sequential enhanced CT in relation to clinical observations. Spine. 1993; 18:843–850.16). Lee KY, Sohn SK, Kim CH, Lee JW. Significans of space-occupying ratio according to MRI finding in lumbar disc herniation. J Kor Spine Surg. 2002; 9:14–18.17). Szypryt EP, Jwining P, Wide GF. Diagnosis of lumbar disc protrusion. J Bone Joint Surg. 1988; 70B:717–722.18). Mink JH. Imaging evaluation of the candidate for percutaneous lumbar discectomy. Clin Orthop. 1989; 238:83–91.
Article19). Powell MC, Wilson M, Szypryt P. Prevalence of lumbar disc degeneration observed magnetic resonance in symp -tomless women. Lancet. 1986; 2:1363–1367.20). Parkkola, M. kormano. Lumbar disc and vack muscle degeneration on MRI: Correlation to age and body mass. J Spinal Disorders. 1992; 5:86–92.21). Williams RW. Microdiskectomy-Myth, mania or mile -stone? An 18 year surgical adventure. The Mount Sinai J of Med. 1991; 58:139–145.22). Wilson D, Harbaugh R. Microsurgical and standard removal of protruded lumbar disc. Acomparative study. Neurosurgery. 1981; 8:422–427.23). Caspar W, Campball B, Barbier DD, Kretschmmer R, Goffried Y. The Caspar microsurgical discectomy and comparison with a conventional standard lumbar disc procedure. Neurosurgery. 1991; 28:78–87.
Article24). Lowell TD, Errico TJ, Fehlings MG, DiBartolo TJ, Ladosi L. Microdiskectomy for lumbar disc herniation: A review of 100cases. Orthopedics. 1995; 18:985–990.25). Balderston RA, Gilyard GG, Jones AM, Wiesel SW, Spengler DM, Bigos SJ, Rothman RH. The treatment of lumbar disc herniation: Simple fragment excision versus disc space curettage. J Spine Disorders. 1991; 4:22–25.26). Williams RW. Result of microsurgery. Williams RW, McCulloch JA, Young PH, editors. Microsurgery of the Lumbar Spine. Rockvill, MD: Aspen;p. 211–214. 1990.27). Koh YD, Kim DJ, Kim JO. Clinical and radilologic factors predicting the low back pain after discectomy. J Kor Spine Surg. 2002; 9:178–183.28). Frymoyer JW. T he adult spine. 2nd ed.Philadelphia: JB L ippincott Co;p. 741–742. 1997.29). Wang JM, Kim DJ. Diagnostic value of image findings of MRI for the internal disc disruption. J Kor Spine Surg. 1997; 4:36–42.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Influence of the Various Configurations of Lower Lumbar and Lumbosacral Spine on the Disc Degeneration: Multifactorial Analysis
- The Changes of Disc Height and Degeneration in Patients with Lumbar Disc Herniation
- Lumbar Disc Degeneration and Segmental Instability: A Comparison of Magnetic Resonance Images and Plain Radiographs
- MRI Assessments of Adjacent Disc Degeneration Following Lumbar Fusion
- Changes of Posterior Bulging of the Lumbar Intervertebral Discs with Flexion and Extension in Central Disc Bulges and Disc Degeneration