J Korean Soc Spine Surg.
2007 Sep;14(3):151-157. 10.4184/jkss.2007.14.3.151.
Treatment Outcome of Reoperative Lumbar Disc Herniation
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, Dong-A University, Busan, Korea. gylee@dau.ac.kr
- KMID: 1941646
- DOI: http://doi.org/10.4184/jkss.2007.14.3.151
Abstract
-
STUDY DESIGN: A retrospective study.
OBJECTIVES
To analyze the causes and treatment outcomes of reoperation after a lumbar discectomy. SUMMARY OF LITERATURE REVIEW: The major causes of reoperation after a lumbar disc surgery is recurrent disc herniation. Satisfactory outcomes can be obtained with reoperation for patients still requiring treatment.
MATERIALS AND METHODS
Fifty two patients, who had undergone reoperations after lumbar discectomies with a minimum followup period of one year, were reviewed. The causes of the reoperation were analyzed according to the physical examination and conventional radiographic evaluation. The surgical outcome was assessed using the JOA score and Kirkaldy-Willis criteria, and the recovery rate was calculated according to the JOA score. Statistical analysis was carried out to evaluate the factors that might influence the outcome of reoperation.
RESULTS
The causes of reoperation after lumbar disc surgery included 46 cases of recurrent disc herniation, each two cases of the wrong level, spinal canal stenosis and lumbar instability. The average JOA score increased from 11 to 24, and the average recovery rate was approximately 72%. According to the Kirkaldy-Willis criteria, the results were excellent and good in approximately 85% of cases. Statistical analysis revealed that the factors associated with a successful outcome were a single previous surgical procedure (p.0.02), a preoperative JOA score over 10 points (p.0.01), and a pain-free interval of more than 12 months after the previous operation(p.0.01).
CONCLUSION
The treatment outcomes of reoperative lumbar disc herniation were satisfactory. Factors, such as the low number of prior procedures, high preoperative JOA score, and long pain-free interval after a previous operation, can lead to a successful treatment outcome of reoperation.
MeSH Terms
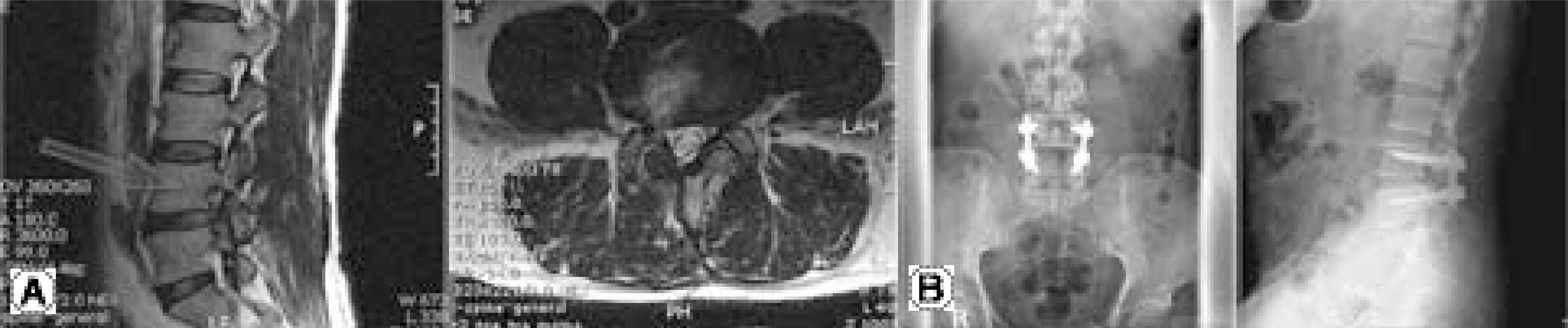
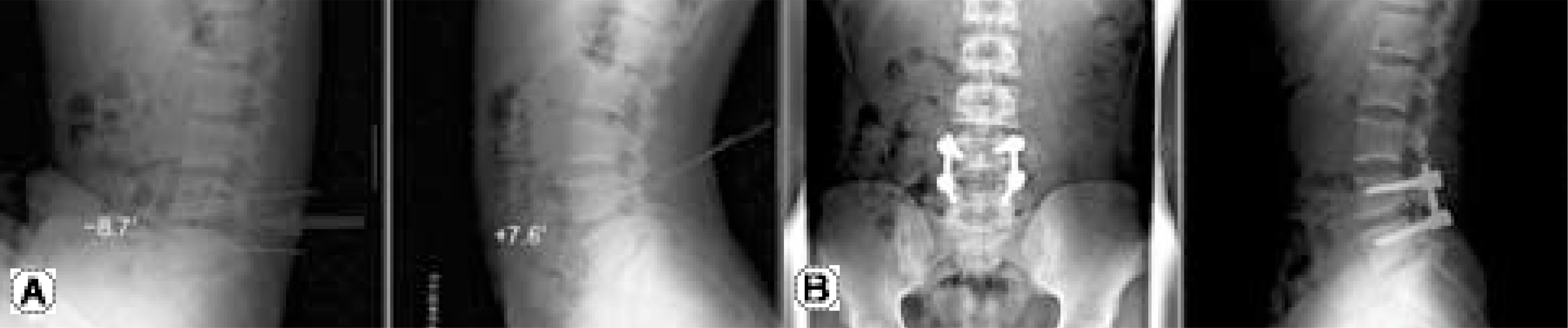
Figure
Reference
-
1). Andrews DW, Lavyne MH. Retrospective analysis of microsurgical and standard lumbar discectomy. Spine. 1990; 15:329–335.
Article2). Barrios C, Ahmed M, Arrotegui J, Bjornsson A, Gill-strom P. Microsurgery versus standard removal of the herniated lumbar disc. Acta Orthop scand. 1990; 61:339–403.3). Dvorak J, Gauchat MH, Valach L. The outcome of surgery for lumbar disc herniation. A 4-17 years' followup with emphasis on somatic aspects. Spine. 1998; 13:1418–1422.4). Eismont FJ, Currier B. Surgical management of lumbar intervertebral disc disease. J bone joint surg Am. 1989; 71:1266–1271.5). Kahanovitz N, Viola K, McCulloch J. Limited surgical discectomy and microdiscectomy. A clinical comparison. Spine. 1989; 14:79–81.6). Weber H. Lumbar disc herniation. A controlled, prospective study with 10 years of observation. Spine. 1983; 8:131–140.7). Bernard TN. Repeat lumbar spine surgery. Factors influ-encing outcome. Spine. 1993; 18:2196–2200.8). Brinckmann P, Grootenboer H. Change of disc height, radial disc bulge, and intradiscal pressure from disecto-my. An in vitro investigation on human lumbar discs. Spine. 1991; 16:641–646.9). Fandino J, Botana C, Viladrich A, Gomez-Bueno J. Reoperation after lumar disc surgery: Results in 130 cases. Acta Neurochir. 1993; 122:102–104.10). Greenwood J, McGuire TH, Kimbel EF. A study of the causes of failure in the herniated intervetebral disc operation. J Neuosurg. 1952; 9:15–20.11). Kim SS, Michelsan CB. Revision surgery for failed back surgery. Spine. 1992; 17:957–960.12). Ashok B, Steven PH, Gunnar BJA. Lumbar disc disease in Rothman-Simeone eds. The spine. 5th ed.Philadelphia: W.B. Saunders Co;p. 930–944. 2006.13). Mixter WJ, Barr JA. Rupture of the intervertebral disc with involvement of the spinal cord. New engl J Med. 1934; 211:210–215.14). O'sullivam MG, Commolly AE, Buckley TF. Recurrent lumbar disc protrusion, Br J Neurosur. 1990; 4:319–325.15). Pappas CTE, Harrinton T, Sonntaf VKH. Outcome analysis in 654 surgically treated lumbar disc herniation. Neurosurgery. 1992; 30:862–866.16). Rish BL. A critique of the surgical management of lumbar disease in a private neurological practice. Spine. 1984; 9:500–504.17). Spanfort EV. The lumbar disc herniaiton, A computer-aided analysis 2,504 operations. Acta Orthop Scand Suppl. 1972; 142:1–95.18). Amstrong JR. The causes of unsatisfactory results from the operative treatment of lumbar disc lesion. J bone joint surg Br. 1951; 33:31–35.19). Fager CA, Friedberg SR. Analysis of failure and poor results of lumbar spine surgery. Spine. 1980; 5:87–94.20). Ford LT. Postoperative infection of intervertebral disc space. South Med J. 1955; 48:1295–1303.
Article21). Spengler DM. Lumbar discectomy. Results with limited disc excison and selective foraminotomy. Spine. 1982; 7:604–607.22). Quimjian JD, Matrka PJ. Decompression laminectomy and lateral spinal fusion in patients with previously failed spine surgery. Orthopedics. 1988; 11:563–569.23). O'sullivan MG, Commolly AE, Buckley TF. Recurrent lumbar disc protrusion, Br J Neurosur. 1990; 4:319–325.24). Cinotti G, Roysam GS, Eisenstein SM, Postacchini F. Ipsilateral recurrent lumbar disc herniation, A prospective controlled study. J Bone Joint Surg Br. 1998; 80:825–832.25). Williams RW. Microlumbar discectomy: A conservative surgical approach to the virgin herniated lumbar disc. Spine. 1978; 3:175–182.26). Ethier DB, Cain JC, Yaszemski MJ, et al. .:. The influence of anulotomy selection on disc competence. Spine. 1994; 19:2071–2076.
Article27). Wiesel SW. The multiply operated lumbar spine. Instructional Course Lecture, AAOS Meeting. 1985; 34:68–77.28). Finnegan WJ, Fenlin FM, Marvel JP, Nardini RJ, Rothman GH. Results of surgical intervention in the symptomatic multiply operated back patient. J Bone Joint surg Am. 1979; 61:1077–1082.29). Waddell G, Kummel EG, McCulloch HA. Failed lumbar disc surgery and repeated surgery following industrial injuries. J bong Joint surg Am. 1979; 61:201–207.30). Pheasan HC. Source of failure in laminectomies. Orthop clin N Am. 1975; 6:319–330.31). Dai LY, Zhou Q, Yao WF, Shen L. Recurrent lumbar disc herniation after discectomy: Outcome of repeat discectomy. Surg Neurol. 2005; 64:226–231.
Article32). Jackson RK. The longterm effects of wide laminectomy for lumbar disc excision, A review of 130 patients. J Bone Joint surg Br. 1971; 53:609–616.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rapid Repeated Recurrent Lumbar Disc Herniation after Microscopic Discectomies
- Clinical Analysis of Recurrent Lumbar Disc Herniation
- Juvenile Lumbar Intervertebral Disc Herniation: Five Cases Report
- Redundant Nerve Roots of Cauda Equina Mimicking Intradural Disc Herniation: A Case Report
- High Lumbar Disc Herniation Treated With an Anterolateral Approach: Case Report