Anat Cell Biol.
2014 Dec;47(4):236-243. 10.5115/acb.2014.47.4.236.
Upper terminal of the inferior vena cava and development of the heart atriums: a study using human embryos
- Affiliations
-
- 1Department of Anatomy, Chonbuk National University Medical School, Jeonju, Korea. 407kk@hanmail.net
- 2Department of Surgery, Daejeon Sun Hospital, Daejeon, Korea.
- 3Institute of Embryology, Universidad Complutense, Madrid, Spain.
- 4Division of Internal Medicine, Iwamizawa Asuka Hospital, Iwamizawa, Japan.
- 5Department of Surgery and Biomedical Research Institute, Chonbuk National University Hospital, Jeonju, Korea.
- KMID: 1882602
- DOI: http://doi.org/10.5115/acb.2014.47.4.236
Abstract
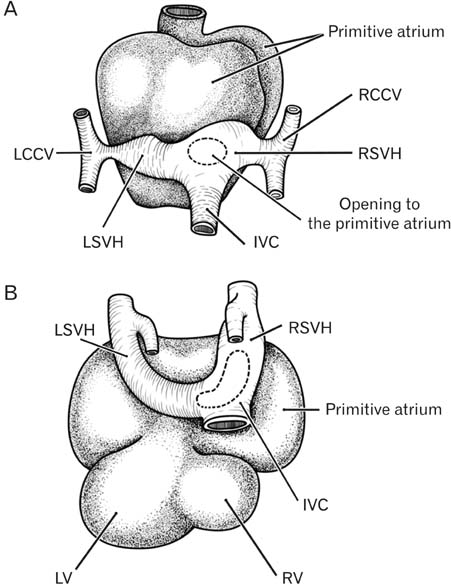
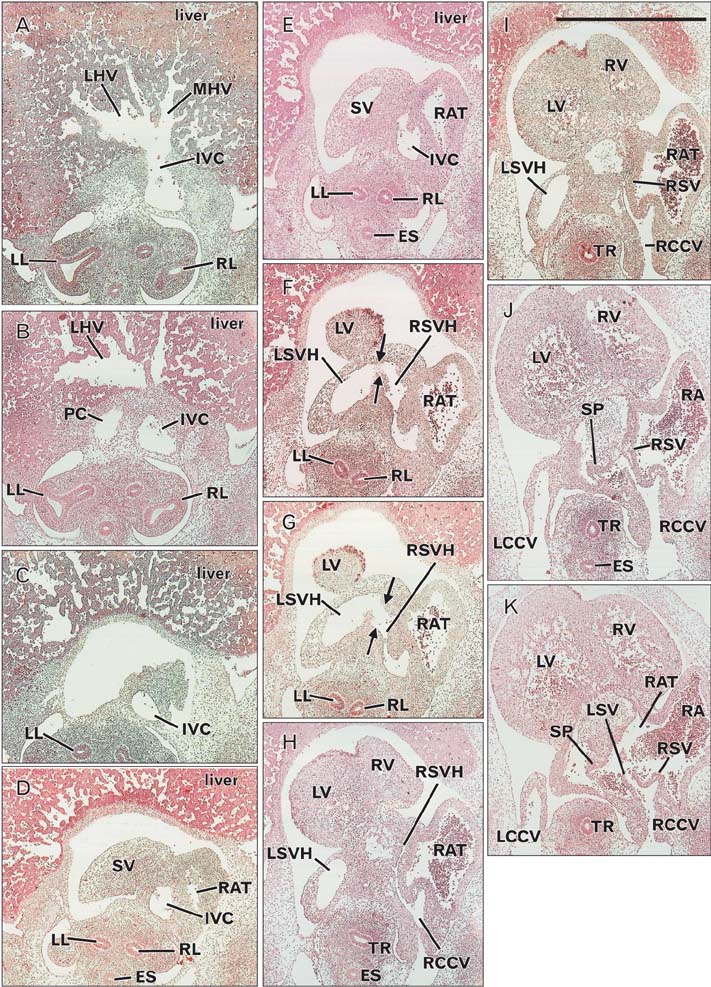
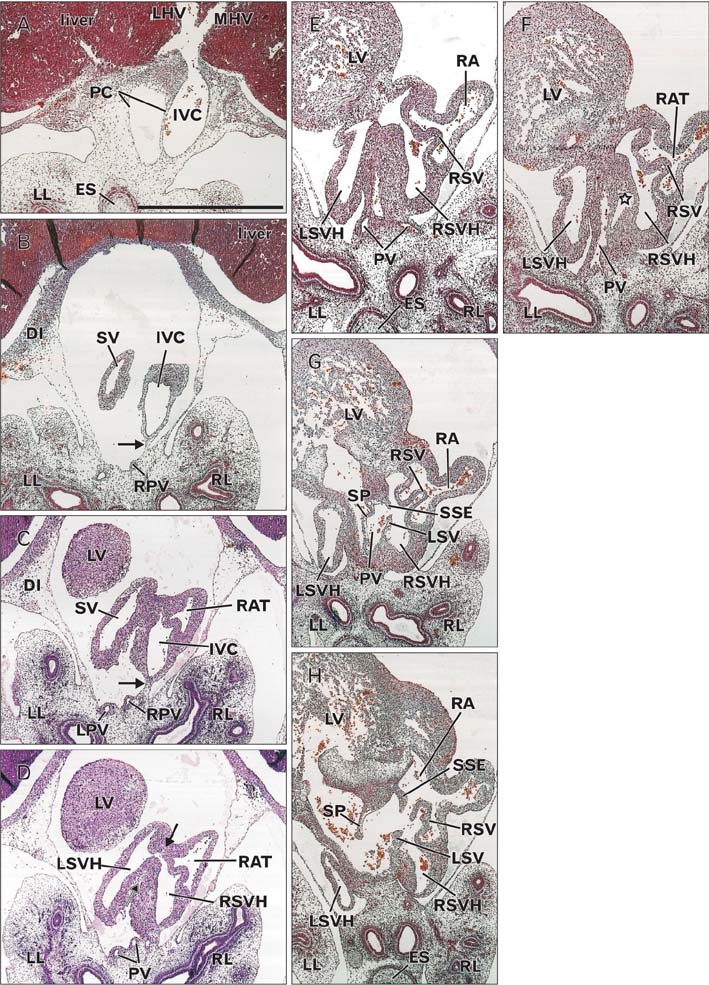
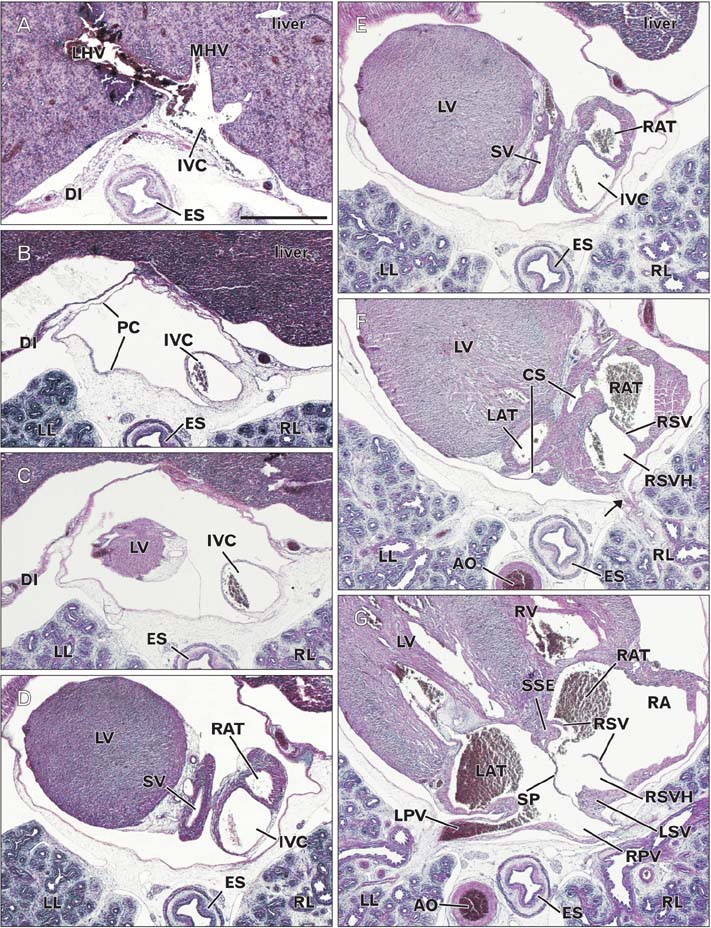
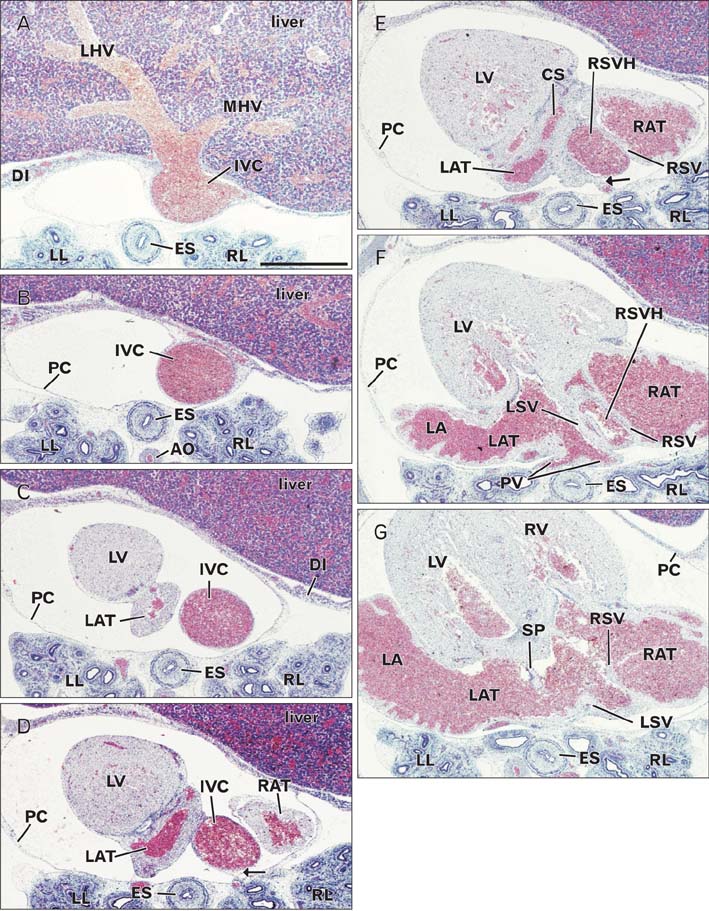
- In the embryonic heart, the primitive atrium is considered to receive the bilateral sinus horns including the upper terminal of the inferior vena cava (IVC). To reveal topographical anatomy of the embryonic venous pole of the heart, we examined horizontal serial paraffin sections of 15 human embryos with crown-rump length 9-31 mm, corresponding to a gestational age of 6-7 weeks or Carnegie stage 14-16. The IVC was often fixed to the developing right pulmonary vein by a mesentery-like fibrous tissue. Rather than the terminal portion of the future superior vena cava, the IVC contributed to form a right-sided atrial lumen at the stage. The sinus venosus or its left horn communicated with the IVC in earlier specimens, but in later specimens, the left atrium extended caudally to separate the sinus and IVC. In contrast, the right atrium consistently extended far caudally, even below the sinus horn, along the IVC. A small (or large) attachment between the left (or right) atrium and IVC in adult hearts seemed to be derived from the left (or right) sinus valve. This hypothesis did not contradict with the incorporation theory of the sinus valves into the atrial wall. Variations in topographical anatomy around the IVC, especially of the sinus valves, might not always depend on the stages but partly in individual differences.
Keyword
MeSH Terms
Figure
Reference
-
1. Anderson RH, Brown NA, Moorman AF. Development and structures of the venous pole of the heart. Dev Dyn. 2006; 235:2–9.2. Sizarov A, Anderson RH, Christoffels VM, Moorman AF. Three-dimensional and molecular analysis of the venous pole of the developing human heart. Circulation. 2010; 122:798–807.3. Dickson AD. The development of the ductus venosus in man and the goat. J Anat. 1957; 91:358–368.4. Mavrides E, Moscoso G, Carvalho JS, Campbell S, Thilaganathan B. The anatomy of the umbilical, portal and hepatic venous systems in the human fetus at 14-19 weeks of gestation. Ultrasound Obstet Gynecol. 2001; 18:598–604.5. Collardeau-Frachon S, Scoazec JY. Vascular development and differentiation during human liver organogenesis. Anat Rec (Hoboken). 2008; 291:614–627.6. Blom NA, Gittenberger-de Groot AC, Jongeneel TH, DeRuiter MC, Poelmann RE, Ottenkamp J. Normal development of the pulmonary veins in human embryos and formulation of a morphogenetic concept for sinus venosus defects. Am J Cardiol. 2001; 87:305–309.7. Steding G, Xu JW, Seidl W, Männer J, Xia H. Developmental aspects of the sinus valves and the sinus venosus septum of the right atrium in human embryos. Anat Embryol (Berl). 1990; 181:469–475.8. Webb S, Kanani M, Anderson RH, Richardson MK, Brown NA. Development of the human pulmonary vein and its incorporation in the morphologically left atrium. Cardiol Young. 2001; 11:632–642.9. Hayashi S, Fukuzawa Y, Rodríguez-Vázquez JF, Cho BH, Verdugo-López S, Murakami G, Nakano T. Pleuroperitoneal canal closure and the fetal adrenal gland. Anat Rec (Hoboken). 2011; 294:633–644.10. Rodríguez-Vázquez JF, Kim JH, Verdugo-López S, Murakami G, Cho KH, Asakawa S, Abe S. Human fetal hyoid body origin revisited. J Anat. 2011; 219:143–149.11. Miyake N, Hayashi S, Kawase T, Cho BH, Murakami G, Fujimiya M, Kitano H. Fetal anatomy of the human carotid sheath and structures in and around it. Anat Rec (Hoboken). 2010; 293:438–445.12. Bartram U, Van Praagh S, Keane JF, Lang P, van der Velde ME, Van Praagh R. Mitral and aortic atresia associated with hypoplastic right lung, crossover segment of right lower lobe, and anomalous scimitar-like right pulmonary venous connection with inferior vena cava: clinical, angiocardiographic, and autopsy findings in a rare case. Pediatr Dev Pathol. 1998; 1:413–419.13. Sadler TW. Langman's medical embryology. 7th ed. Baltimore: Williams & Wilkins;1995.14. Moore KL, Persaud TV. The developing human: clinically oriented embryology. 6th ed. Philadelphia: W. B. Saunders;1998.