Diabetes Metab J.
2011 Oct;35(5):513-522. 10.4093/dmj.2011.35.5.513.
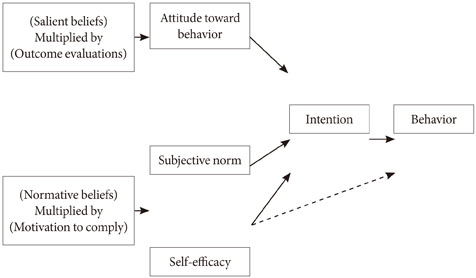
Factors Influencing Physical Activity Behavior among Iranian Women with Type 2 Diabetes Using the Extended Theory of Reasoned Action
- Affiliations
-
- 1Department of Health and Social Medicine, Urmia University of Medical Sciences, School of Medicine, Urmia, Iran.
- 2Department of Health Education, Tehran University of Medical Sciences, School of Public Health, Tehran, Iran. shojaee@sina.tums.ac.ir
- 3Department of Health Education, Tarbiat Modares University, School of Medical Sciences, Tehran, Iran.
- 4Department of Biostatistics, Tarbiat Modares University, School of Medical Sciences, Tehran, Iran.
- 5Department of Nutrition and Biochemistry, Urmia University of Medical Sciences, School of Medicine, Urmia, Iran.
- KMID: 1857507
- DOI: http://doi.org/10.4093/dmj.2011.35.5.513
Abstract
- BACKGROUND
Findings of most studies indicate that the only way to control diabetes and prevent its debilitating effects is through the continuous performance of self-care behaviors. Physical activity is a non-pharmacological method of diabetes treatment and because of its positive effects on diabetic patients, it is being increasingly considered by researchers and practitioners. This study aimed at determining factors influencing physical activity among diabetic women in Iran, using the extended theory of reasoned action in Iran.
METHODS
A sample of 352 women with type 2 diabetes, referring to a Diabetes Clinic in Khoy, Iran, participated in the study. Appropriate instruments were designed to measure the desired variables (knowledge of diabetes, personal beliefs, subjective norms, perceived self-efficacy, behavioral intention and physical activity behavior). The reliability and validity of the instruments were examined and approved. Statistical analyses of the study were conducted by inferential statistical techniques (independent t-test, correlations and regressions) using the SPSS package.
RESULTS
The findings of this investigation indicated that among the constructs of the model, self efficacy was the strongest predictor of intentions among women with type 2 diabetes and both directly and indirectly affected physical activity. In addition to self efficacy, diabetic patients' physical activity also was influenced by other variables of the model and sociodemographic factors.
CONCLUSION
Our findings suggest that the high ability of the theory of reasoned action extended by self-efficacy in forecasting and explaining physical activity can be a base for educational intervention. Educational interventions based on the proposed model are necessary for improving diabetics' physical activity behavior and controlling disease.
MeSH Terms
Figure
Reference
-
1. Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010. 87:4–14.2. Delavari A, Mahdavi-Hezaveh A, Noroozinajad A, Yarahmadi SH. A national design for the prevention and control of diabetes. 2004. Tehran: Disease Management Center, Ministry of Health and Medical Education, Iran.3. 2005 National diabetes fact sheet. Centers for Disease Control and Prevention. accessed 2006 June 1. Available from: http://www.cdc.gov/diabetes/pubs/estimates05.htm#prev.4. Lim S, Kim DJ, Jeong IK, Son HS, Chung CH, Koh G, Lee DH, Won KC, Park JH, Park TS, Ahn J, Kim J, Park KG, Ko SH, Ahn YB, Lee I. A nationwide survey about the current status of glycemic control and complications in diabetic patients in 2006: The Committee of the Korean Diabetes Association on the Epidemiology of Diabetes Mellitus. Korean Diabetes J. 2009. 33:48–57.5. Gochman DS. Chapter 6, The history and meaning of patient compliance as an ideology. Handbook of health behavior research, II. Provider determinants. 1997. New York: Plenum Press;109–124.6. Sechrist KR, Walker SN, Pender NJ. Development and psychometric evaluation of the exercise benefits/barriers scale. Res Nurs Health. 1987. 10:357–365.7. Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Canadian Diabetes Association 2003 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes. 2003. 27:Suppl 2. S1–S152.8. Bhaskarabhatla KV, Birrer R. Physical activity and type 2 diabetes: tailoring exercise to optimize fitness and glycemic control. Phys Sportsmed. 2004. 32:13–17.9. Larijani B. Exercise and diabetes. 2003. Tehran: Tehran University of Medical Sciences;13.10. Ford ES, Herman WH. Leisure-time physical activity patterns in the U.S. diabetic population. Findings from the 1990 National Health Interview Survey--Health Promotion and Disease Prevention Supplement. Diabetes Care. 1995. 18:27–33.11. Costanzo C, Walker SN, Yates BC, McCabe B, Berg K. Physical activity counseling for older women. West J Nurs Res. 2006. 28:786–801.12. Yamaguchi Y, Miura S, Urata H, Himeshima Y, Yamatsu K, Otsuka N, Nishida S, Saku K. The effectiveness of a multicomponent program for nutrition and physical activity change in clinical setting: short-term effect of PACE+ Japan. Int J Sport Health Sci. 2003. 1:229–237.13. Nutbeam D, Harris E. Theory in a nutshell: a practical guide to health promotion theories. 2004. 2nd ed. Sydney: McGraw-Hill.14. Kulh J, Beckman J. Action control: from cognition to behavior. 1985. Heildberg: Springer;11–39. From intentions to actions: a theory of planned behavior.15. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977. 84:191–215.16. Godin G, Kok G. The theory of planned behavior: a review of its applications to health-related behaviors. Am J Health Promot. 1996. 11:87–98.17. Strecher VJ, DeVellis BM, Becker MH, Rosenstock IM. The role of self-efficacy in achieving health behavior change. Health Educ Q. 1986. 13:73–92.18. Brinson D. The self-management of type2 diabetes: changing exercise behaviors for better health [master's thesis]. 2007. Christchurch: University of Canterbury;296–298.19. Rothman AJ. Toward a theory-based analysis of behavioral maintenance. Health Psychol. 2000. 19:1 Suppl. 64–69.20. Bandura A. Self-efficacy mechanism in human agency. Am Psychol. 1982. 37:122–147.21. Francis JJ, Eccles MP, Johnston M, Walker A, Grimshaw J, Foy R, Kaner EF, Smith L, Bonetti D. Constructing questionnaires based on the theory of planned behaviour: a manual for health services researchers. 2004. Newcastle upon Tyne: Centre for Health Services Research, University of Newcastle;1–40.22. Ajzen I: Constructing a TPB questionnaire: conceptual and methodological considerations. cited 2011 Jul 26. Available from: http://www.people.umass.edu/aizen/contact.html.23. Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000. 23:943–950.24. Rovniak LS, Anderson ES, Winett RA, Stephens RS. Social cognitive determinants of physical activity in young adults: a prospective structural equation analysis. Ann Behav Med. 2002. 24:149–156.25. Giles M, McClenahan C, Cairns E, Mallet J. An application of the theory of planned behaviour to blood donation: the importance of self-efficacy. Health Educ Res. 2004. 19:380–391.26. Norman P, Hoyle S. The theory of planned behavior and breast self-examination: distinguishing between perceived control and self-efficacy. J Appl Soc Psychol. 2004. 34:694–708.27. Ma WF, Lane HY, Laffrey SC. A model testing factors that influence physical activity for Taiwanese adults with anxiety. Res Nurs Health. 2008. 31:476–489.28. Walker SN, Pullen CH, Hertzog M, Boeckner L, Hageman PA. Determinants of older rural women's activity and eating. West J Nurs Res. 2006. 28:449–468.29. Omondi DO, Walingo MK, Mbagaya GM, Othuon LO. Understanding physical activity behavior of type 2 diabetics using the theory of planned behavior and structural equation modeling. Int J Hum Soc Sci. 2010. 5:160–167.30. Blue CL. Does the theory of planned behavior identify diabetes-related cognitions for intention to be physically active and eat a healthy diet? Public Health Nurs. 2007. 24:141–150.31. Trost SG, Saunders R, Ward DS. Determinants of physical activity in middle school children. Am J Health Behav. 2002. 26:95–102.32. Symons Downs D, Hausenblas HA. The theories of reasoned action and planned behavior applied to exercise: a meta-analytic update. J Phys Act Health. 2005. 2:76–97.33. Bozionelos G, Bennett P. The theory of planned behavior as predictor of exercise: the moderating influence of beliefs and personality variables. J Health Psychol. 1999. 4:517–529.34. Fishbein M, Ajzen I. Belief, attitude, intention and behavior: an introduction to theory and research. 1975. Menlo Park: Addison-Wesley;15–45.35. Van Ryn M, Lytle LA, Kirscht JP. A test of the theory of planned behavior for two health-related practices. J Appl Soc Psychol. 1996. 26:817–883.36. Surit P. Health beliefs, social support, and self-care of behaviors of older Thai persons with non-insulin-dependent diabetes mellitus (NIDDM) [dissertation]. 2001. Washington, DC: Catholic University of America.37. Baum A, Newman S, Weinman J, West R, McManus C. Theory of planned behavior. Cambridge handbook of psychology, health and medicine. 1997. Cambridge: Cambridge University Press;177–179.38. Jiang YD, Chuang LM, Wu HP, Shiau SJ, Wang CH, Lee YJ, Juang JH, Lin BJ, Tai TY. Assessment of the function and effect of diabetes education programs in Taiwan. Diabetes Res Clin Pract. 1999. 46:177–182.39. Chan YM, Molassiotis A. The relationship between diabetes knowledge and compliance among Chinese with non-insulin dependent diabetes mellitus in Hong Kong. J Adv Nurs. 1999. 30:431–438.40. Salmon J, Owen N, Bauman A, Schmitz MK, Booth M. Leisure-time, occupational, and household physical activity among professional, skilled, and less-skilled workers and homemakers. Prev Med. 2000. 30:191–199.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Related to the Health Behavior of Urban Residents on the Basis of Theory of Reasoned Action
- Health-Related Behaviors: Theoretical Models And Research Findings
- A Study on the Sociopsychological Factors Influencing the Dietary Compliance of Diabetics Using Questionnaire
- Testing the Theory of Planned Behavior in the Prediction and Intention of Smoking Cessation Behavior
- Factors Influencing Physical Activity among Community-dwelling Older Adults with Type 2 Diabetes: A Path Analysis