Korean J Urol.
2012 Oct;53(10):691-698. 10.4111/kju.2012.53.10.691.
Ultrasound Characteristics of Patients with Urinary Stress Incontinence with or without Genital Prolapse
- Affiliations
-
- 1Department for Urogynaecology and Pelvic Floor Disorders, University Clinic for Gynaecology and Obstetrics, Medical Faculty, University "Saint Cyril and Methodius", Skopje, Republic of Macedonia, Europe. www.vantovska@yahoo.com
- KMID: 1856988
- DOI: http://doi.org/10.4111/kju.2012.53.10.691
Abstract
- PURPOSE
The study purpose was to evaluate the clinical and ultrasound characteristics of women with urinary stress incontinence (USI) with or without genital prolapse (GP).
MATERIALS AND METHODS
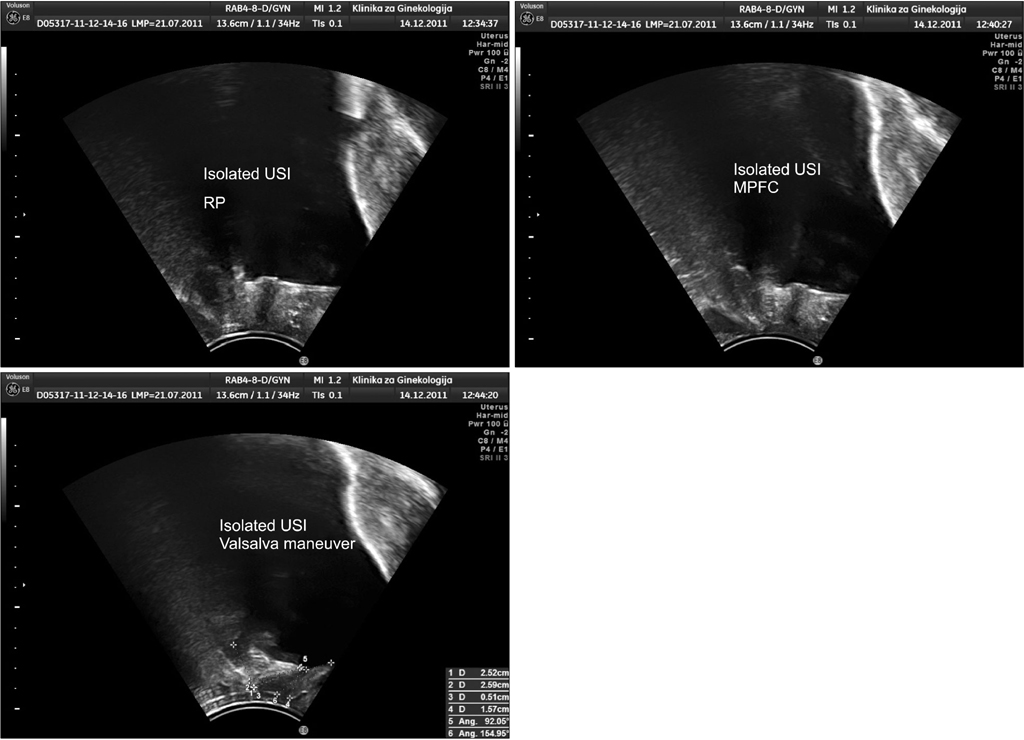
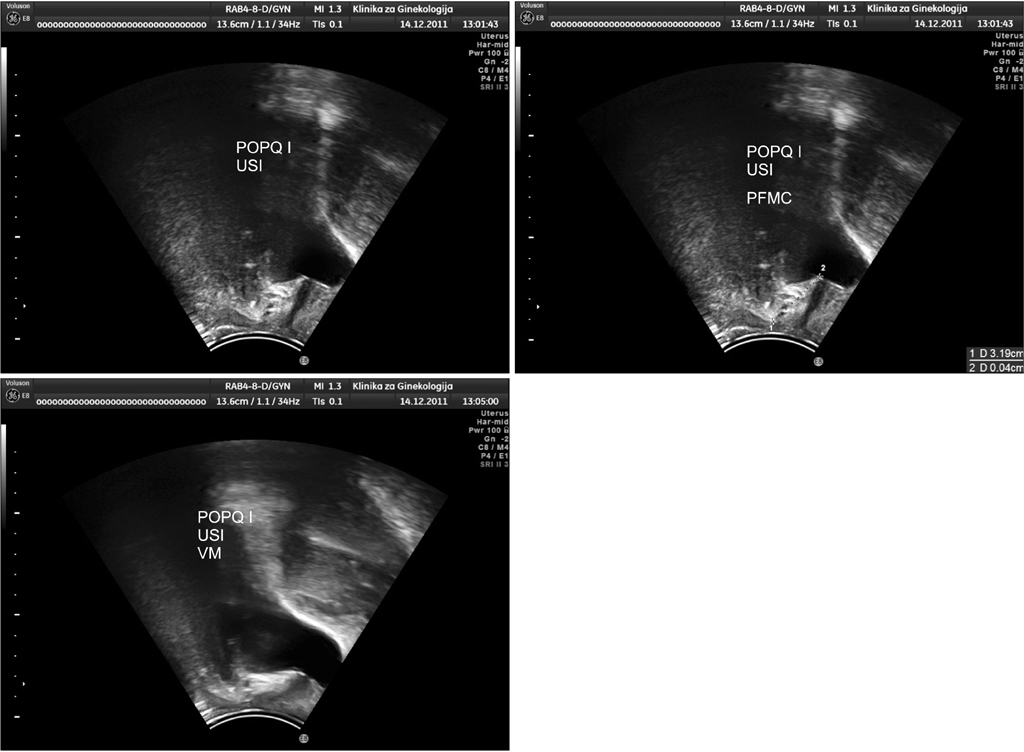
A total of 268 patients who underwent ultrasound perineal evaluation were divided into two groups: isolated USI (n=132) and USIGP (n=136) with USI/GP stage I/II. The latter group was additionally divided into two subgroups: USIGP(A) (n=78) with USI/GP stage I and USIGP(B) (n=58) with USI/GP stage II.
RESULTS
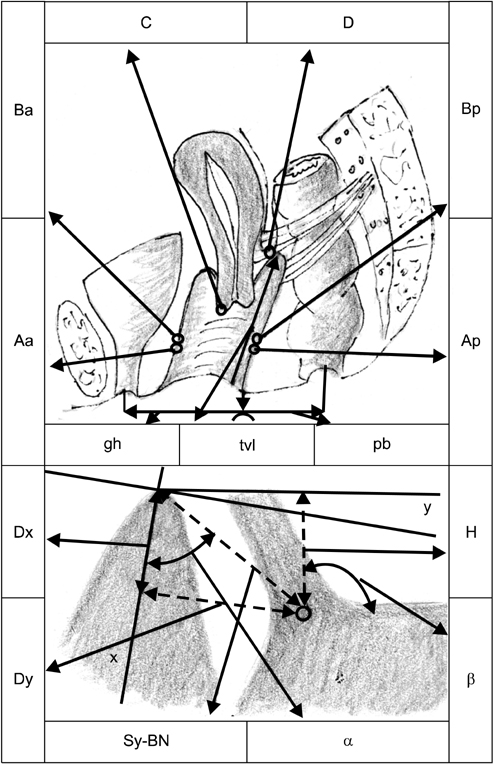
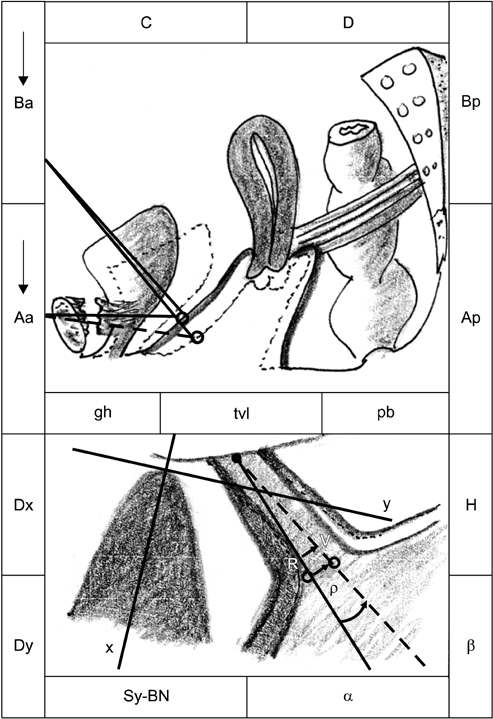
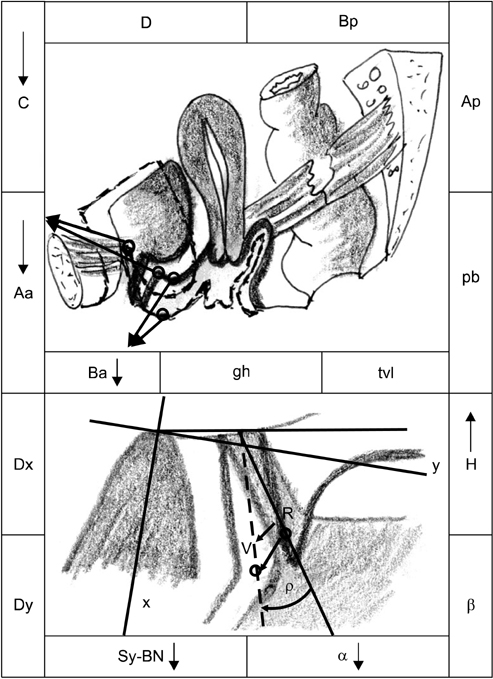
Point Aa (pelvic organ prolapse quantification system), which is the projection of the bladder neck (BN) on the anterior vaginal wall, was situated higher in the rest position (RP) but moved lower during a Valsalva maneuver (VM) in the USI group than in the USIGP group (p<0.05). The ultrasound parameters alpha-angle and the distance Sy-BN (symphisis-bladder neck) decreased, whereas distance H increased, in the USIGP group during VM. The ultrasound parameters that gave the best insight into the range of BN movements were as follows: distance R-->V and angle of rotation (rho), which were significantly higher in the USI group than in the USIGP group during VM.
CONCLUSIONS
According to the clinical and ultrasound findings, we can conclude that the BN is situated higher during the RP but moved lower during a VM in patients with isolated USI compared with those with concomitant USI/GP, which could be explained by the cystocele-immobilizing effect on the BN during the VM in the latter group but also by the deteriorated pubo-urethral ligaments in the former group.
MeSH Terms
Figure
Reference
-
1. Schaer G, Koelbl H, Voigt R, Merz E, Anthuber C, Niemeyer R, et al. Recommendations of the German Association of Urogynecology on functional sonography of the lower female urinary tract. Int Urogynecol J Pelvic Floor Dysfunct. 1996. 7:105–108.2. Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996. 175:10–17.3. Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet. 2001. 357:1191–1194.4. Abrams P, Blaivas JG, Stanton SL, Andersen JT. The International Continence Society Committee on Standardisation of Terminology. The standardisation of terminology of lower urinary tract function. Scand J Urol Nephrol Suppl. 1988. 114:5–19.5. Chen HY, Huang YL, Hung YC, Chen WC. Evaluation of stress urinary incontinence by computer-aided vector-based perineal ultrasound. Acta Obstet Gynecol Scand. 2006. 85:1259–1264.6. Thompson JA, O'Sullivan PB, Briffa NK, Neumann P. Comparison of transperineal and transabdominal ultrasound in the assessment of voluntary pelvic floor muscle contractions and functional manoeuvres in continent and incontinent women. Int Urogynecol J Pelvic Floor Dysfunct. 2007. 18:779–786.7. Bai SW, Kwon JY, Chung da J, Park JH, Kim SK. Differences in urodynamic study, perineal sonography and treatment outcome according to urethrovesical junction hypermobility in stress urinary incontinence. J Obstet Gynaecol Res. 2006. 32:206–211.8. Huang WC, Yang SH, Yang JM. Anatomical and functional significance of urogenital hiatus in primary urodynamic stress incontinence. Ultrasound Obstet Gynecol. 2006. 27:71–77.9. Dietz HP. The role of two- and three-dimensional dynamic ultrasonography in pelvic organ prolapse. J Minim Invasive Gynecol. 2010. 17:282–294.10. Hajebrahimi S, Azaripour A, Sadeghi-Bazargani H. Clinical and transperineal ultrasound findings in females with stress urinary incontinence versus normal controls. Pak J Biol Sci. 2009. 12:1434–1437.11. Minardi D, Piloni V, Amadi A, El Asmar Z, Milanese G, Muzzonigro G. Correlation between urodynamics and perineal ultrasound in female patients with urinary incontinence. Neurourol Urodyn. 2007. 26:176–182.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidence of Concomitant Procedures for Pelvic Organ Prolapse and Reconstruction in Women Who Undergo Sling Operation for Stress Urinary Incontinence
- Current Trends in the Surgical Management of Stress Urinary Incontinence and Pelvic Organ Prolapse
- Measurement of Postvoid Residual Volume in Advanced Pelvic Organ Prolapse Classified by Pelvic Organ Prolapse Quantification[POP-Q]
- Letter to the editor: Comment on "Simultaneous treatment of anterior vaginal wall prolapse and stress urinary incontinence by using transobturator four arms polypropylene mesh"
- The authors reply: Simultaneous treatment of anterior vaginal wall prolapse and stress urinary incontinence by using transobturator four arms polypropylene mesh