Tuberc Respir Dis.
2012 Dec;73(6):325-330. 10.4046/trd.2012.73.6.325.
A Case of Radiation Bronchitis Induced Massive Hemoptysis after High-Dose-Rate Endobronchial Brachytherapy
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea. wonylee@yonsei.kr
- 2Department of Radiation Oncology, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 3Department of Pathology, Yonsei University Wonju College of Medicine, Wonju, Korea.
- KMID: 1842926
- DOI: http://doi.org/10.4046/trd.2012.73.6.325
Abstract
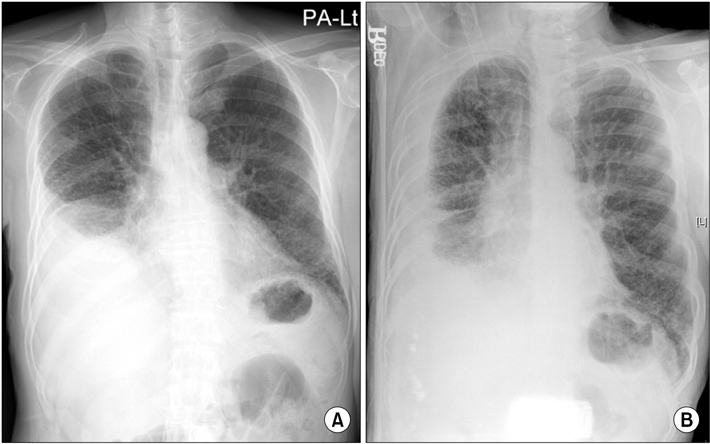
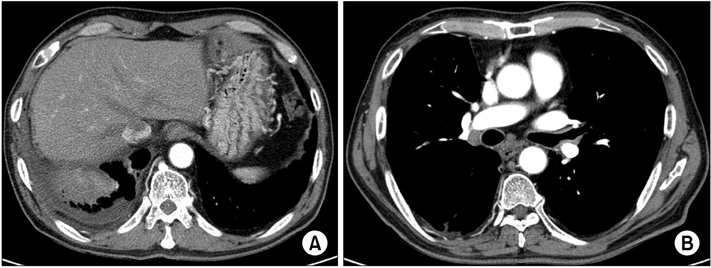
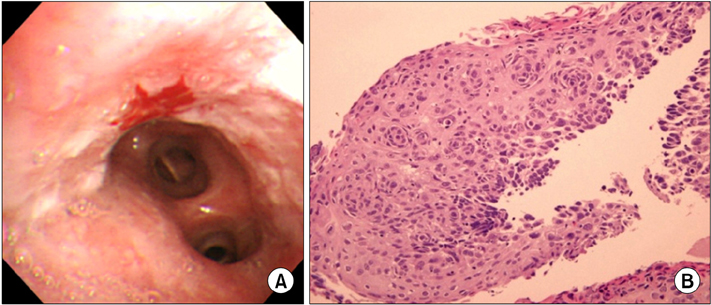
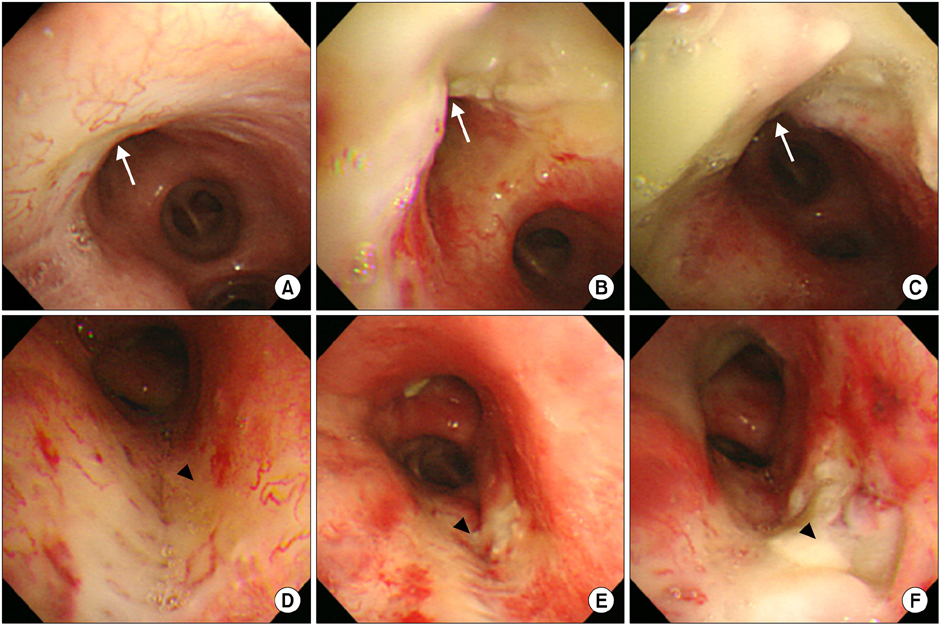
- High-dose-rate endobronchial brachytherapy (HDREB) have been used as the treatment of early endobronchial cancer, as well as for palliation of advanced cancer. However, fatal hemoptysis can occur after HDREB at the rate of 7~32%. We report a case of massive hemoptysis due to radiation bronchitis developed after HDREB. A 67-year-old man was treated with HDREB for early endobronchial cancer on the left upper lobe bronchus. He complained of persistent cough from 4 weeks after completion of HDREB. Radiation bronchitis was observed on the bronchoscopy at 34 weeks, and it was progressed from mucosal swelling and exudate formation to necrosis and ulceration without local relapse. In addition, he died of massive hemoptysis after 15 months. The patient had no sign or radiologic evidences to predict the hemoptysis. This case implies that HDREB directly contributes to an occurrence of a fatal hemoptysis, and follow-up bronchoscopy is important to predict a progression of radiation bronchitis and fatal hemoptysis.
Keyword
MeSH Terms
Figure
Reference
-
1. Bedwinek J, Petty A, Bruton C, Sofield J, Lee L. The use of high dose rate endobronchial brachytherapy to palliate symptomatic endobronchial recurrence of previously irradiated bronchogenic carcinoma. Int J Radiat Oncol Biol Phys. 1992. 22:23–30.2. Ozkok S, Karakoyun-Celik O, Goksel T, Mogulkoc N, Yalman D, Gok G, et al. High dose rate endobronchial brachytherapy in the management of lung cancer: response and toxicity evaluation in 158 patients. Lung Cancer. 2008. 62:326–333.3. Marsiglia H, Baldeyrou P, Lartigau E, Briot E, Haie-Meder C, Le Chevalier T, et al. High-dose-rate brachytherapy as sole modality for early-stage endobronchial carcinoma. Int J Radiat Oncol Biol Phys. 2000. 47:665–672.4. Hennequin C, Bleichner O, Trédaniel J, Quero L, Sergent G, Zalcman G, et al. Long-term results of endobronchial brachytherapy: a curative treatment? Int J Radiat Oncol Biol Phys. 2007. 67:425–430.5. Aumont-le Guilcher M, Prevost B, Sunyach MP, Peiffert D, Maingon P, Thomas L, et al. High-dose-rate brachytherapy for non-small-cell lung carcinoma: a retrospective study of 226 patients. Int J Radiat Oncol Biol Phys. 2011. 79:1112–1116.6. Hara R, Itami J, Aruga T, Kozuka T, Nakajima K, Yamashita H, et al. Risk factors for massive hemoptysis after endobronchial brachytherapy in patients with tracheobronchial malignancies. Cancer. 2001. 92:2623–2627.7. Hennequin C, Tredaniel J, Chevret S, Durdux C, Dray M, Manoux D, et al. Predictive factors for late toxicity after endobronchial brachytherapy: a multivariate analysis. Int J Radiat Oncol Biol Phys. 1998. 42:21–27.8. Gollins SW, Ryder WD, Burt PA, Barber PV, Stout R. Massive haemoptysis death and other morbidity associated with high dose rate intraluminal radiotherapy for carcinoma of the bronchus. Radiother Oncol. 1996. 39:105–116.9. Chung MP, Kwon OJ, Choi DR, Huh SJ, Lim DH, Kim MK, et al. Short-term results of endobronchial brachytherapy for malignant airway obstructions. J Korean Soc Ther Radiol. 1996. 14:299–306.10. Park YJ, Kim CY, Kim KT, Yang DS, Lee S. The palliative effect of endobronchial brachytherapy for previously irradiated patients with lung cancer. J Korean Soc Ther Radiol Oncol. 2007. 25:177–184.11. Speiser BL, Spratling L. Radiation bronchitis and stenosis secondary to high dose rate endobronchial irradiation. Int J Radiat Oncol Biol Phys. 1993. 25:589–597.12. Taulelle M, Chauvet B, Vincent P, Félix-Faure C, Buciarelli B, Garcia R, et al. High dose rate endobronchial brachytherapy: results and complications in 189 patients. Eur Respir J. 1998. 11:162–168.13. Edell ES, Cortese DA. Bronchoscopic phototherapy with hematoporphyrin derivative for treatment of localized bronchogenic carcinoma: a 5-year experience. Mayo Clin Proc. 1987. 62:8–14.14. Maiwand MO, Asimakopoulos G. Cryosurgery for lung cancer: clinical results and technical aspects. Technol Cancer Res Treat. 2004. 3:143–150.15. Matsumoto I, Oda M, Imagawa T, Yachi T, Fujimori H, Watanabe G. Management of tracheobronchial ulceration induced by high-dose brachytherapy. Ann Thorac Surg. 2009. 87:1301–1303.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endobronchial Brachytherapy for MalignantAirway Obstruction: Low Dose Rate Versus High Dose Rate
- Endobronchial Brachytherapy of Advanced Non-small Cell Lung Carcinoma
- Short-term Results of Endobronchial Brachytherapy for Malignant Airway Obstructions
- The Effects of High Dose Rate Brachytherapy in Recurrent Obstructive Bronchogenic Cancer after External Irradiation Therapy
- Second Line Palliative Endobronchial Radiotherapy with HDR Ir 192 in Recurrent Lung Carcinoma