Korean Circ J.
2009 May;39(5):205-208. 10.4070/kcj.2009.39.5.205.
Very Late Thrombosis of a Drug-Eluting Stent After Discontinuation of Dual Antiplatelet Therapy in a Patient Treated With Both Drug-Eluting and Bare-Metal Stents
- Affiliations
-
- 1The Heart Center of Chonnam National University Hospital, Gwangju, Korea. myungho@chollian.net
- 2Cardiovascular Research Institute of Chonnam National University, Gwangju, Korea.
- KMID: 1826020
- DOI: http://doi.org/10.4070/kcj.2009.39.5.205
Abstract
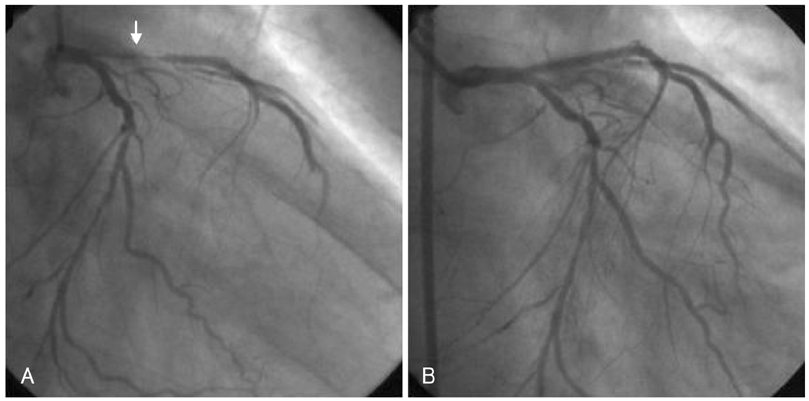
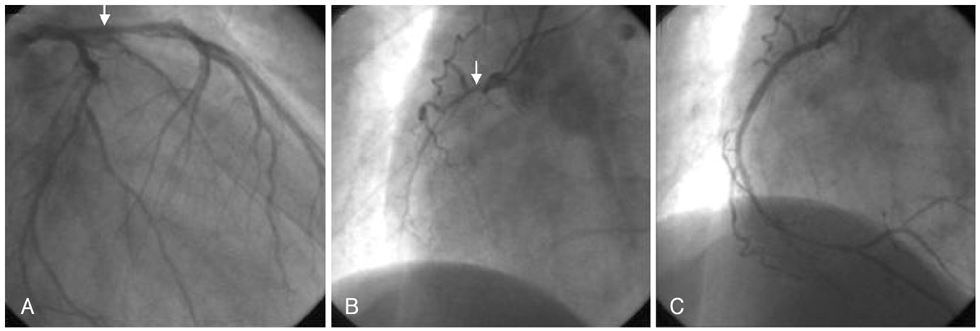
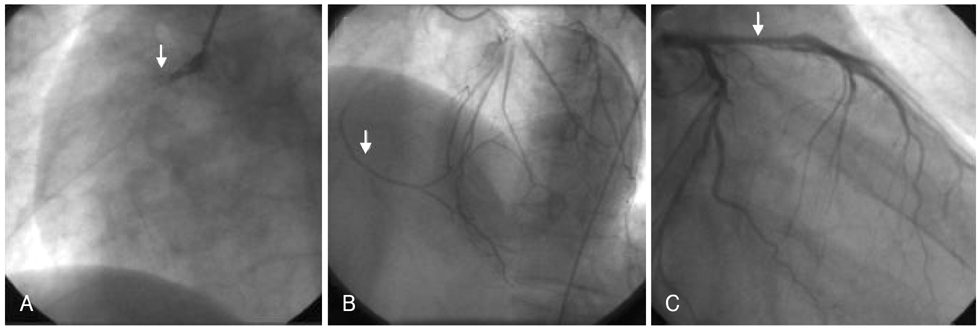
- Drug-eluting stents (DESs) are the treatment of choice for obstructive coronary artery disease when percutaneous intervention is feasible. However, late stent thrombosis seems to occur more frequently with DESs and is closely associated with the discontinuation of dual antiplatelet therapy. We report a case of very late stent thrombosis after discontinuation of dual antiplatelet therapy. The patient suffered from acute myocardial infarction (MI) and underwent bare metal stent (BMS) implantation in the left anterior descending artery (LAD) five years prior to presentation. Three years after BMS implantation, he presented again with acute MI and had a DES implanted in the right coronary artery (RCA). He ran out of his medication, but failed to refill his prescription. Sixteen days after discontinuing medication, he experienced an episode of chest pain and was taken to the cardiac catheterization laboratory, where he was found to have thrombosis in the DES, but no thrombosis in the BMS. It is possible that DESs are more vulnerable to late thrombosis than are BMSs, supporting the use of prolonged dual antiplatelet therapy in patients treated with DESs. The patient was successfully treated with balloon angioplasty and thrombus aspiration without complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Serruys PW, Degertekin M, Tanabe K, et al. Intravascular ultrasound findings in the multicenter, randomized, double-blind RAVEL (Randomized study with the sirolimus-eluting Velocity balloon-expandable stent in the treatment of patients with de novo native coronary artery Lesions) trial. Circulation. 2002. 106:798–803.2. Colombo A, Drzewiecki J, Banning A, et al. Randomized study to assess the effectiveness of slow- and moderate-release polymer-based paclitaxel-eluting stents for coronary artery lesions. Circulation. 2003. 108:788–794.3. Zhang F, Ge J, Qian J, et al. Sirolimus-eluting stents in real-world patients with ST-segment elevation acute myocardial infarction. Int Heart J. 2007. 48:303–311.4. Daemen J, Wenaweser P, Tsuchida K, et al. Early and late coronary stent thrombosis of sirolimus-eluting and paclitaxel-eluting stents in routine clinical practice: data from a large two-institutional cohort study. Lancet. 2007. 369:667–678.5. Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007. 115:2344–2351.6. Bavry AA, Kumbhani DJ, Helton TJ, et al. Late thrombosis of drug-eluting stents: a meta-analysis of randomized clinical trials. Am J Med. 2006. 119:1056–1061.7. Mauri L, Hsieh WH, Massaro JM, et al. Stent thrombosis in randomized clinical trials of drug-eluting stents. N Engl J Med. 2007. 356:1020–1029.8. Kuchulakanti PK, Chu WW, Torguson R, et al. Correlates and long-term outcomes of angiographically proven stent thrombosis with sirolimus- and paclitaxel-eluting stents. Circulation. 2006. 113:1108–1113.9. Park SH, Hong GR, Seo HS, Tahk SJ. Stent thrombosis after successful drug-eluting stent implantation. Korean Circ J. 2005. 35:163–171.10. Iakovou I, Schmidt T, Bonizzouni E, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug eluting stents. JAMA. 2005. 293:2126–2130.11. Flores-Rios X, Marzoa-Rivas R, Abugattás-de Torres JP, et al. Late thrombosis of paclitaxel-eluting stents: long-term incidence, clinical consequences, and risk factors in a cohort of 604 patients. Am Heart J. 2008. 155:648–653.12. Pfisterer M, Brunner-La Rocca HP, Buser PT, et al. Late clinical events after clopidogrel discontinuation may limit the benefit of drug-eluting stents: an observational study of drug-eluting versus bare-metal stents. J Am Coll Cardiol. 2006. 48:2584–2591.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Stent Thrombosis Occurred at 5 Years after Sirolimus-Eluting Stent Implantation
- Stent Thrombosis in the Era of the Drug-Eluting Stent
- A Case of Neointimal Calcification in a Drug-Eluting Stent
- A Case of Ticagrelor Rescue Therapy in a Patient with Subacute Stent Thrombosis
- Very Late Stent Thrombosis Related to Fracture of a Sirolimus-Eluting Stent