Yonsei Med J.
2010 Jul;51(4):534-539. 10.3349/ymj.2010.51.4.534.
Case Review of Impacted Bile Duct Stone at Duodenal Papilla: Detection and Endoscopic Treatment
- Affiliations
-
- 1Department of Internal Medicine, Kyung Hee University School of Medicine, Seoul, Korea. krjoo@khu.ac.kr
- 2Department of Surgery, Kyung Hee University School of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- KMID: 1805190
- DOI: http://doi.org/10.3349/ymj.2010.51.4.534
Abstract
- PURPOSE
A bile duct stone impacted at the duodenal papilla is an urgent condition that can rapidly lead to either suppurative cholangitis or acute pancreatitis due to almost complete obstruction of the bilio-pancreatic outflow. This study evaluated the clinical characteristics and results of endoscopic treatment for a bile duct stone impacted at the duodenal papilla.
MATERIALS AND METHODS
Forty-six patients who had been diagnosed with an impacted papillary stone were retrospectively reviewed.
RESULTS
The typical features of acute cholangitis (Charcot's triad) and pancreatitis were only observed only in 10 patients (21.7%) and 17 patients (37.0%), respectively. After the endoscopic retrograde cholangiopancreatography, 30 patients (65.2%) were found to have a solitary stone impacting the duodenal papilla and 16 patients had one or more stones in the bile duct. On the radiological studies, the former patients were associated more commonly with no visible stone or no bile duct dilatation (p < 0.05). All impacted papillary stones were successfully removed by endoscopic sphincterotomy: 23 by a needle knife and 23 by a pull type papillotome. The procedure-related complications (n = 7, 4 bleeding, 3 pancreatitis) were not serious and did not differ, based on endoscopic findings and the procedure used.
CONCLUSION
A bile duct stone impacted at the duodenal papilla requires both clinical and radiographic evidence to support the diagnosis. Endoscopic sphincterotomy, either with a needle knife or a pull type papillotome, was safe and effective for removing the impacted papillary stone.
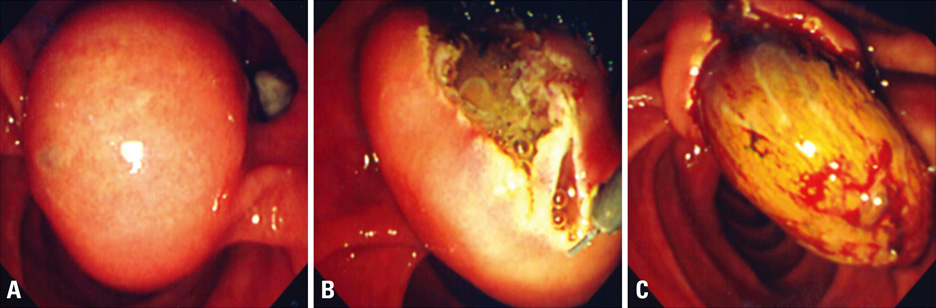
Figure
Reference
-
1. Leung JW, Banez VP, Chung SC. Precut (needle knife) papillotomy for impacted common bile duct stone at the ampulla. Am J Gastroenterol. 1990. 85:991–993.2. Binmoeller KF, Katon RM. Needle knife papillotomy for an impacted common bile duct stone during pregnancy. Gastrointest Endosc. 1990. 36:607–609.
Article3. Heinerman PM, Boeckl O, Pimpl W. Selective ERCP and preoperative stone removal in bile duct surgery. Ann Surg. 1989. 209:267–272.
Article4. Freitas ML, Bell RL, Duffy AJ. Choledocholithiasis: evolving standards for diagnosis and management. World J Gastroenterol. 2006. 12:3162–3167.5. Cotton PB, Vallon AG. British experience with duodenoscopic sphincterotomy for removal of bile duct stones. Br J Surg. 1981. 68:373–375.6. Siegel JH. Precut papillotomy: a method to improve success of ERCP and papillotomy. Endoscopy. 1980. 12:130–133.7. Akcakaya A, Ozkan OV, Okan I, Kocaman O, Sahin M. Endoscopic retrograde cholangiopancreatography during pregnancy without radiation. World J Gastroenterol. 2009. 15:3649–3652.
Article8. McAlister VC, Roy A, Passi RB. Harpoon extraction of a common bile duct stone impacted at the ampulla of Vater with needle-knife sphincterotome. Gastrointest Endosc. 1993. 39:111–112.
Article9. Conio M, Saccomanno S, Aste H, Pugliese V. Precut papillotomy: primum non nocere. Gastrointest Endosc. 1990. 36:544.
Article10. Siegel JH, Ben-Zvi JS, Pullano W. The needle knife: a valuable tool in diagnostic and therapeutic ERCP. Gastrointest Endosc. 1989. 35:499–503.11. Kozarek RA, Sanowski RA. Endoscopic choledochoduodenostomy. Gastrointest Endosc. 1983. 29:119–121.12. Schapira L, Khawaja FI. Endoscopic fistulo-sphincterotomy: an alternative method of sphincterotomy using a new sphincterotome. Endoscopy. 1982. 14:58–60.13. Kim DI, Kim MH, Lee SK, Seo DW, Choi WB, Lee SS, et al. Risk factors for recurrence of primary bile duct stones after endoscopic biliary sphincterotomy. Gastrointest Endosc. 2001. 54:42–48.
Article14. Tytgat GN. The Sydney System: endoscopic division. Endoscopic appearances in gastritis/duodenitis. J Gastroenterol Hepatol. 1991. 6:223–234.
Article15. Rajnakova A, Goh PM, Ngoi SS, Lim SG. ERCP in patients with periampullary diverticulum. Hepatogastroenterology. 2003. 50:625–628.16. Lobo DN, Balfour TW, Iftikhar SY. Periampullary diverticula: consequences of failed ERCP. Ann R Coll Surg Engl. 1998. 80:326–331.17. Vaira D, Dowsett JF, Hatfield AR, Cairns SR, Polydorou AA, Cotton PB, et al. Is duodenal diverticulum a risk factor for sphincterotomy? Gut. 1989. 30:939–942.
Article18. Cotton PB. Endoscopic management of bile duct stones; (apples and oranges). Gut. 1984. 25:587–597.19. Kirk AP, Summerfield JA. Incidence and significance of juxtapapillary diverticula at endoscopic retrograde cholangiopancreatography. Digestion. 1980. 20:31–35.20. Osnes M, Kahrs T. Endoscopic choledochoduodenostomy for choledocholithiasis through choledochoduodenal fistula. Endoscopy. 1977. 9:162–165.21. Wang P, Li ZS, Liu F, Ren X, Lu NH, Fan ZN, et al. Risk factors for ERCP-related complications: a prospective multicenter study. Am J Gastroenterol. 2009. 104:31–40.22. Williams EJ, Taylor S, Fairclough P, Hamlyn A, Logan RF, Martin D, et al. Risk factors for complication following ERCP; results of a large-scale, prospective multicenter study. Endoscopy. 2007. 39:793–801.
Article23. Cotton PB. Precut papillotomy--a risky technique for experts only. Gastrointest Endosc. 1989. 35:578–579.
Article24. Kim HJ, Kim MH, Kim DI, Lee HJ, Myung SJ, Yoo KS, et al. Endoscopic hemostasis in sphincterotomy-induced hemorrhage: its efficacy and safety. Endoscopy. 1999. 31:431–436.
Article25. Park JS, Kim MH, Lee SK, Seo DW, Lee SS, Chang HS, et al. The clinical significance of papillitis of the major duodenal papilla. Gastrointest Endosc. 2002. 55:877–882.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Application of Clips during ERCP: A New Anchoring Method for Redundant Kerckrings Folds Covering the Duodenal Papilla
- A Case of Anomalous Termination of the Common Bile Duct and the Pancreatic Duct into the Duodenal Bulb, Associated with Common Bile Duct Stones
- Clinical Features of Impacted Common Bile Duct Stones at Duodenal Papilla
- Pancreatic and Biliary Strictures Associated with Cholangitis and Bile Reflux Following Endoscopic Papillectomy of Ampullary Adenoma
- Ectopic Opening of the Common Bile Duct into the Duodenal Bulb: A Case Report