Yonsei Med J.
2014 Sep;55(5):1253-1259. 10.3349/ymj.2014.55.5.1253.
Surgical Experience with Infective Endocarditis and Aortic Root Abscess
- Affiliations
-
- 1Division of Cardiovascular Surgery, Severance Cardiovascular Hospital, Department of Thoracic and Cardiovascular Surgery, Yonsei University College of Medicine, Seoul, Korea. HANK@yuhs.ac
- KMID: 1799488
- DOI: http://doi.org/10.3349/ymj.2014.55.5.1253
Abstract
- PURPOSE
This study was conducted to evaluate the surgical outcomes of active infective endocarditis with aortic root abscess formation.
MATERIALS AND METHODS
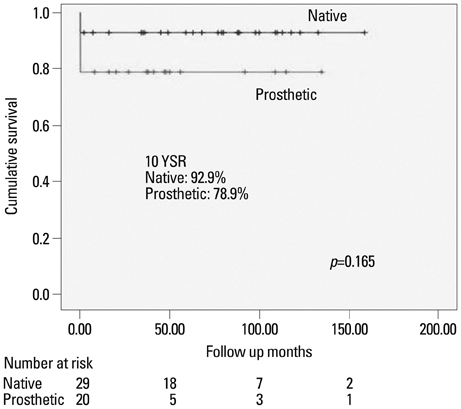
Between February 1999 and June 2012, 49 patients underwent surgery for active endocarditis with aortic root abscess. The infected valve was native in 29 patients and prosthetic in 20 patients. The patients' mean age was 50+/-14 years, and 36 patients were male. Surgery was urgent/emergent in 15 patients (31%). The abscess involved the aortic annulus (11), left ventricular outflow tract (18), fibrous trigone (16), and mitral annulus (4). In all patients, wide debridement of abscess and aortic valve replacement with or without patch reconstruction of aortic root or annulus was performed.
RESULTS
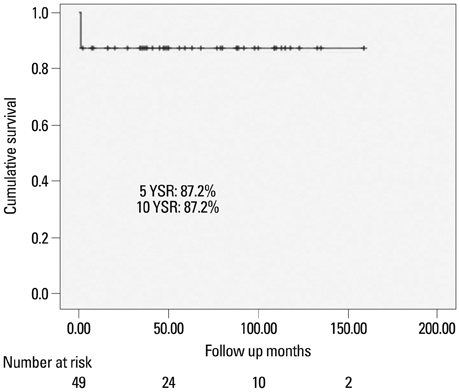
There were 6 (12%) operative deaths. Causes of early mortality were sepsis (2) and multi-organ failure (4). On postoperative echocardiogram, there was significant improvement of left ventricular dimension (LVEDD, from 58.8+/-11.8 mm to 52.6+/-8.2 mm, p<0.001); however, LV ejection fraction was significantly decreased (from 61.4+/-12.0% to 49.8+/-16.5%, p<0.001). The mean follow-up duration was 68.7+/-40.4 months. There was no late death or recurrent endocarditis during follow up. New York Heart Association functional class significantly improved from 3.2+/-0.7 to 1.2+/-0.4 (p<0.001). Kaplan-Meier estimated survival at 10 years was 87.2%.
CONCLUSION
Surgical treatment for active endocarditis with aortic root abscess is still challenging, and was associated with high operative mortality. Nevertheless, long-term survival was excellent with good functional capacity after recovery from the early postoperative period.
Keyword
MeSH Terms
-
Abscess/*surgery
Adult
Aortic Valve/microbiology/*surgery
Debridement
Endocarditis/*surgery
Female
Follow-Up Studies
Heart Valve Prosthesis/*microbiology
Heart Valve Prosthesis Implantation/*adverse effects/mortality
Humans
Intraoperative Complications/epidemiology
Kaplan-Meier Estimate
Male
Middle Aged
Postoperative Complications/epidemiology
Retrospective Studies
Figure
Reference
-
1. David TE, Regesta T, Gavra G, Armstrong S, Maganti MD. Surgical treatment of paravalvular abscess: long-term results. Eur J Cardiothorac Surg. 2007; 31:43–48.
Article2. Hill EE, Herijgers P, Herregods MC, Peetermans WE. Evolving trends in infective endocarditis. Clin Microbiol Infect. 2006; 12:5–12.
Article3. Heiro M, Helenius H, Mäkilä S, Hohenthal U, Savunen T, Engblom E, et al. Infective endocarditis in a Finnish teaching hospital: a study on 326 episodes treated during 1980-2004. Heart. 2006; 92:1457–1462.
Article4. Leontyev S, Borger MA, Modi P, Lehmann S, Seeburger J, Doenst T, et al. Surgical management of aortic root abscess: a 13-year experience in 172 patients with 100% follow-up. J Thorac Cardiovasc Surg. 2012; 143:332–337.
Article5. Hori D, Noguchi K, Nomura Y, Tanaka H. Perivalvular pseudoaneurysm caused by streptococcus dysgalactiae in the presence of prosthetic aortic valve endocarditis. Ann Thorac Cardiovasc Surg. 2012; 18:262–265.
Article6. Choi SI, Shin DH, Shin JH, Lee JU, Kim SK, Kim KS, et al. A case of aortic root abscess causing fatal myocardial infarction. J Cardiovasc Ultrasound. 2006; 14:63–66.
Article7. Ling LF, To AC, Menon V. Staphylococcus aureus endocarditis complicated by aortic root abscess, coronary fistula, and mitral valve perforation. J Am Coll Cardiol. 2012; 59:e31.
Article8. Parish LM, Liu L, Woo YJ. Endocarditis with massive aortic root abscess and atrioventricular septal destruction. Interact Cardiovasc Thorac Surg. 2009; 8:280–282.
Article9. d'Udekem Y, David TE, Feindel CM, Armstrong S, Sun Z. Long-term results of operation for paravalvular abscess. Ann Thorac Surg. 1996; 62:48–53.10. Daniel WG, Mügge A, Martin RP, Lindert O, Hausmann D, Nonnast-Daniel B, et al. Improvement in the diagnosis of abscesses associated with endocarditis by transesophageal echocardiography. N Engl J Med. 1991; 324:795–800.
Article11. Nakatani S, Mitsutake K, Ohara T, Kokubo Y, Yamamoto H, Hanai S, et al. Recent picture of infective endocarditis in Japan-lessons from Cardiac Disease Registration (CADRE-IE). Circ J. 2013; 77:1558–1564.12. David TE. The surgical treatment of patients with prosthetic valve endocarditis. Semin Thorac Cardiovasc Surg. 1995; 7:47–53.13. David TE, Kuo J, Armstrong S. Aortic and mitral valve replacement with reconstruction of the intervalvular fibrous body. J Thorac Cardiovasc Surg. 1997; 114:766–771.
Article14. David TE, Feindel CM, Armstrong S, Sun Z. Reconstruction of the mitral anulus. A ten-year experience. J Thorac Cardiovasc Surg. 1995; 110:1323–1332.15. Brecker SJ, Pepper JR, Eykyn SJ. Aortic root abscess. Heart. 1999; 82:260–262.
Article16. Iwakura K. Current profile of infective endocarditis in Japan. Circ J. 2013; 77:1411–1413.
Article17. Ishikawa S, Kawasaki A, Neya K, Abe K, Suzuki H, Koizumi S, et al. Surgical treatments for infective endocarditis involving valve annulus. Ann Thorac Cardiovasc Surg. 2009; 15:378–381.18. Perrotta S, Aljassim O, Jeppsson A, Bech-Hanssen O, Svensson G. Survival and quality of life after aortic root replacement with homografts in acute endocarditis. Ann Thorac Surg. 2010; 90:1862–1867.
Article19. Musci M, Weng Y, Hübler M, Amiri A, Pasic M, Kosky S, et al. Homograft aortic root replacement in native or prosthetic active infective endocarditis: twenty-year single-center experience. J Thorac Cardiovasc Surg. 2010; 139:665–673.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Experience of Aortic Root Abscess with Complete AV Block and Pseudoaneurysm
- A Case of Staphylococcal Tricuspid Valve Endocarditis With Para-Aortic Abscess in a Patient With Bicuspid Aortic Valve
- A Case of Aortic Root Abscess Causing Fatal Myocardial Infarction
- Detection of Perivalvular Abscess with Late Gadolinium-Enhanced MR Imaging in a Patient with Infective Endocarditis
- An Aortic Root Abscess Presenting as a Suprasternal Pulsatile Mass