Korean J Ophthalmol.
2014 Feb;28(1):91-95. 10.3341/kjo.2014.28.1.91.
Macular Hole Formation after Pars Plana Vitrectomy for the Treatment of Valsalva Retinopathy: A Case Report
- Affiliations
-
- 1Department of Ophthalmology, Kyung Hee University Hospital, Kyung Hee University School of Medicine, Seoul, Korea. hwkwak@khu.ac.kr
- 2Department of Ophthalmology, Kangwon National University School of Medicine, Chuncheon, Korea.
- KMID: 1792099
- DOI: http://doi.org/10.3341/kjo.2014.28.1.91
Abstract
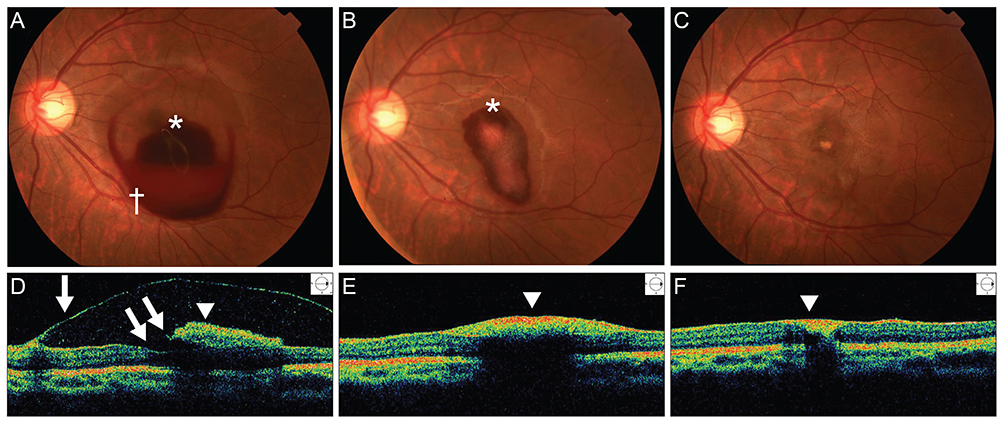
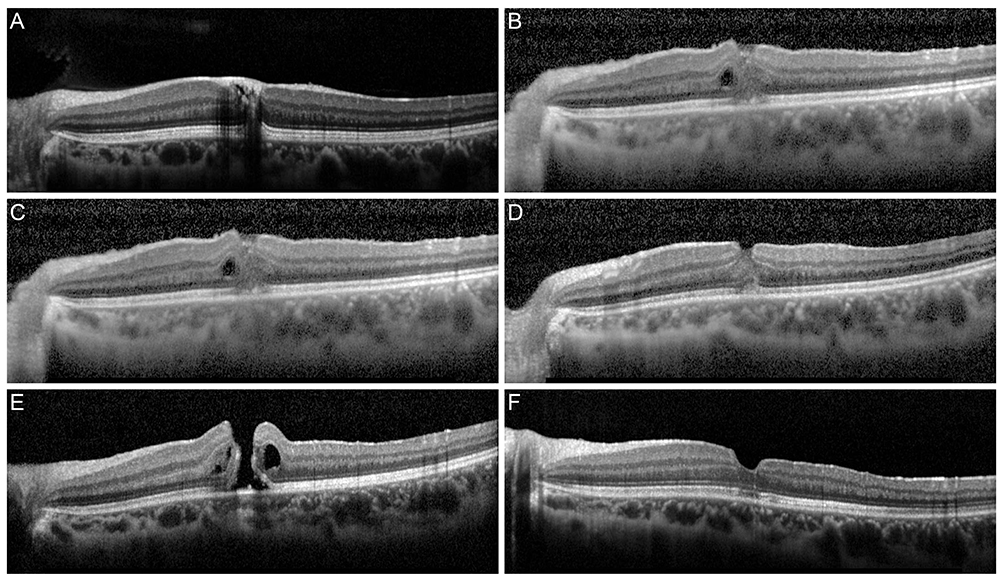
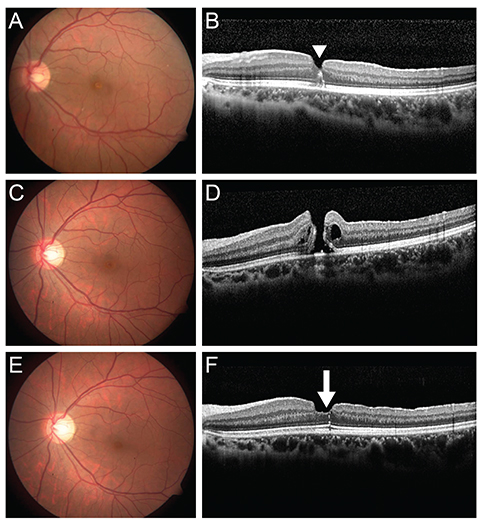
- We report a case of complete surgical resolution of Valsalva retinopathy that manifested as a premacular hemorrhage involving a membrane followed by a macular hole (MH) resulting from the first vitrectomy. A 20-year-old female patient was referred to our hospital due to sudden vision loss in the left eye. Her best-corrected visual acuity (BCVA) in the left eye was hand motion. Fundus photographs and optical coherence tomography (OCT) revealed a premacular hemorrhage. Nine weeks later, the BCVA in the left eye had returned to 20 / 100 and the premacular hemorrhage had completely resolved, but residual sub-internal limiting membrane deposits and a preretinal membrane were present. The preretinal membrane was removed by core vitrectomy and preretinal membrane peeling, but the foveal deposits could not be excised. Two weeks after the first vitrectomy, the deposits resolved spontaneously, but a full-thickness MH was present. Six months after a second vitrectomy with fluid-gas exchange, the BCVA in the left eye had improved to 20 / 25 and OCT showed that the MH had closed. This case illustrates the possibility of MH formation following vitrectomy for Valsalva retinopathy.
Keyword
MeSH Terms
Figure
Reference
-
1. Duane TD. Valsalva hemorrhagic retinopathy. Am J Ophthalmol. 1973; 75:637–642.2. Gass JD. Stereoscopic atlas of macular diseases: diagnosis and treatment. 4th ed. St. Louis: Mosby;1997. p. 752–754.3. Roberts DK, MacKay KA. Microhemorrhagic maculopathy associated with aerobic exercise. J Am Optom Assoc. 1987; 58:415–418.4. Friberg TR, Braunstein RA, Bressler NM. Sudden visual loss associated with sexual activity. Arch Ophthalmol. 1995; 113:738–742.5. De Crecchio G, Pacente L, Alfieri MC, Greco GM. Valsalva retinopathy associated with a congenital retinal macrovessel. Arch Ophthalmol. 2000; 118:146–147.6. Choi SW, Lee SJ, Rah SH. Valsalva retinopathy associated with fiberoptic gastroenteroscopy. Can J Ophthalmol. 2006; 41:491–493.7. Kwok AK, Lai TY, Chan NR. Epiretinal membrane formation with internal limiting membrane wrinkling after Nd:YAG laser membranotomy in valsalva retinopathy. Am J Ophthalmol. 2003; 136:763–766.8. De Maeyer K, Van Ginderdeuren R, Postelmans L, et al. Sub-inner limiting membrane haemorrhage: causes and treatment with vitrectomy. Br J Ophthalmol. 2007; 91:869–872.9. Durukan AH, Kerimoglu H, Erdurman C, et al. Long-term results of Nd:YAG laser treatment for premacular subhyaloid haemorrhage owing to Valsalva retinopathy. Eye (Lond). 2008; 22:214–218.10. Koh HJ, Kim SH, Lee SC, Kwon OW. Treatment of subhyaloid haemorrhage with intravitreal tissue plasminogen activator and C3F8 gas injection. Br J Ophthalmol. 2000; 84:1329–1330.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vitreous Surgery for Macular Hole
- The Clinical Evaluation of Pars Plana Vitrectomy in various Ocular Disease
- Pars Plana Vitrectomy in Pars Planitis and Posterior Uveitis
- Pars Plana Vitrectomy in Pars Planitis and Posterior Uveitis
- Delayed Sealing of Macular Hole after Vitrectomy with Silicone Oil Tamponade