J Korean Med Sci.
2013 Mar;28(3):489-492. 10.3346/jkms.2013.28.3.489.
Utility of F-18 FDG-PET in Detecting Primary Aldosteronism in Patients with Bilateral Adrenal Incidentalomas
- Affiliations
-
- 1Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea. es10@unitel.co.kr
- 2Department of General Surgery, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- 3Department of Pathology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- KMID: 1786952
- DOI: http://doi.org/10.3346/jkms.2013.28.3.489
Abstract
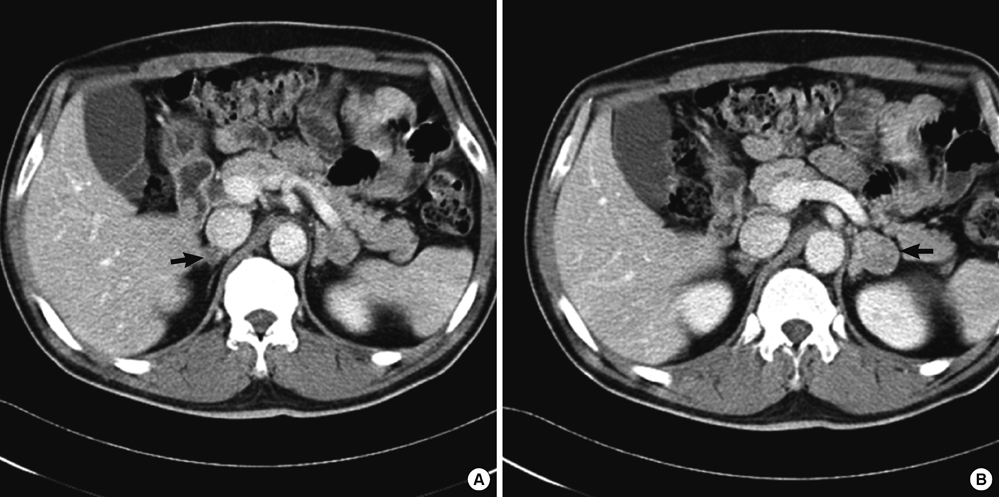
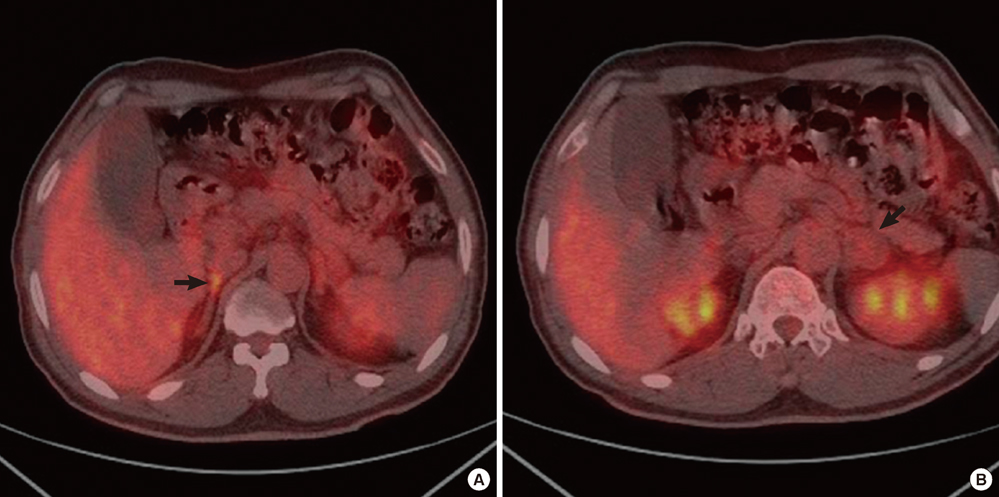
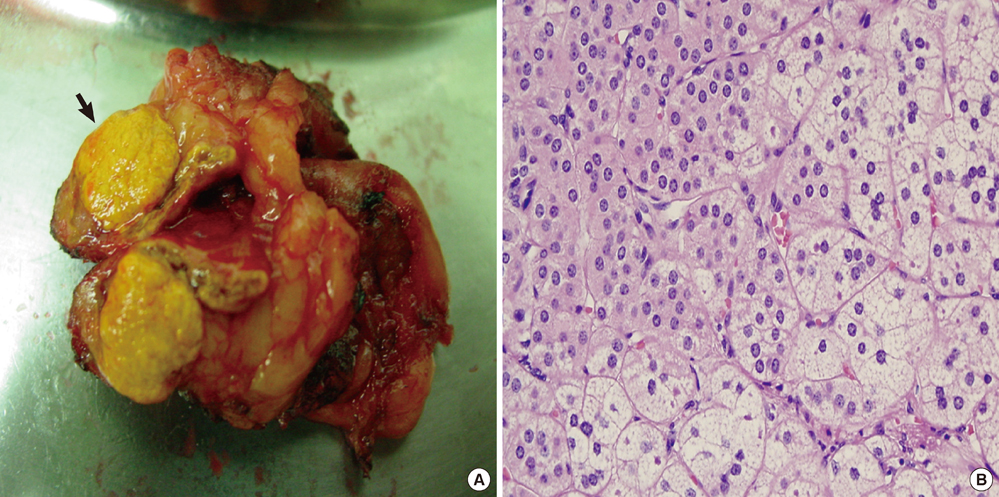
- In patients with primary aldosteronism who have bilateral adrenal incidentalomas, it is important to identify which adrenal gland is secreting excess aldosterone. Traditionally, adrenal vein sampling (AVS) has been performed for lateralization despite its invasiveness. Here we report a case of bilateral adrenal incidentaloma in which 18-Fluorodeoxyglucose (FDG)-positron emission tomography (PET) was used to identify the functional adrenal mass. A 53-yr-old man was referred to our clinic due to bilateral adrenal incidentalomas (right: 1 cm, left: 2.5 cm) on computed tomography (CT). Given his history of colon cancer, FDG-PET/CT scanning was used to rule out metastasis. Although there was focal hot uptake lesion in the right adrenal gland, the patient was suspected primary aldosteronism clinically more than metastasis because of the patient's underlying hypertension with hypokalemia. It was consistent with the results of AVS. Based on these findings, we propose that FDG-PET/CT can be used instead of AVS to identify the source of primary aldosteronism between two bilateral adrenal incidentalomas.
MeSH Terms
-
Adrenal Gland Neoplasms/*diagnosis/pathology/radionuclide imaging
Adrenal Glands/pathology/surgery
Fluorodeoxyglucose F18/diagnostic use
Humans
Hyperaldosteronism/*diagnosis/pathology
Hypertension/diagnosis
Hypokalemia/diagnosis
Male
Middle Aged
Positron-Emission Tomography and Computed Tomography
Fluorodeoxyglucose F18
Figure
Reference
-
1. Barzon L, Boscaro M. Diagnosis and management of adrenal incidentalomas. J Urol. 2000. 163:398–407.2. Kloos RT, Gross MD, Francis IR, Korobkin M, Shapiro B. Incidentally discovered adrenal masses. Endocr Rev. 1995. 16:460–484.3. Jansen PM, Boomsma F, van den Meiracker AH. Dutch ARRAT Investigators. Aldosterone-to-renin ratio as a screening test for primary aldosteronism: the Dutch ARRAT Study. Neth J Med. 2008. 66:220–228.4. Rossi GP. Medscape. A comprehensive review of the clinical aspects of primary aldosteronism. Nat Rev Endocrinol. 2011. 7:485–495.5. Young WF Jr. Clinical practice: the incidentally discovered adrenal mass. N Engl J Med. 2007. 356:601–610.6. Toniato A, Bernante P, Rossi GP, Pelizzo MR. The role of adrenal venous sampling in the surgical management of primary aldosteronism. World J Surg. 2006. 30:624–627.7. Al-Hawary MM, Francis IR, Korobkin M. Non-invasive evaluation of the incidentally detected indeterminate adrenal mass. Best Pract Res Clin Endocrinol Metab. 2005. 19:277–292.8. Han SJ, Kim TS, Jeon SW, Jeong SJ, Yun M, Rhee Y, Kang ES, Cha BS, Lee EJ, Lee HC, et al. Analysis of adrenal masses by 18F-FDG positron emission tomography scanning. Int J Clin Pract. 2007. 61:802–809.9. Ansquer C, Scigliano S, Mirallié E, Taïeb D, Brunaud L, Sebag F, Leux C, Drui D, Dupas B, Renaudin K, et al. 18F-FDG PET/CT in the characterization and surgical decision concerning adrenal masses: a prospective multicentre evaluation. Eur J Nucl Med Mol Imaging. 2010. 37:1669–1678.10. Boland GW, Blake MA, Holalkere NS, Hahn PF. PET/CT for the characterization of adrenal masses in patients with cancer: qualitative versus quantitative accuracy in 150 consecutive patients. AJR Am J Roentgenol. 2009. 192:956–962.11. Wong KK, Arabi M, Zerizer I, Al-Nahhas A, Rubello D, Gross MD. Role of positron emission tomography/computed tomography in adrenal and neuroendocrine tumors: fluorodeoxyglucose and nonfluorodeoxyglucose tracers. Nucl Med Commun. 2011. 32:764–781.12. Burton TJ, Mackenzie IS, Balan K, Koo B, Bird N, Soloviev DV, Azizan EA, Aigbirhio F, Gurnell M, Brown MJ. Evaluation of the sensitivity and specificity of (11)C-metomidate positron emission tomography (PET)-CT for lateralizing aldosterone secretion by Conn's adenomas. J Clin Endocrinol Metab. 2012. 97:100–109.13. Shimizu A, Oriuchi N, Tsushima Y, Higuchi T, Aoki J, Endo K. High [18F] 2-fluoro-2-deoxy-D-glucose (FDG) uptake of adrenocortical adenoma showing subclinical Cushing's syndrome. Ann Nucl Med. 2003. 17:403–406.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of idiopathic hyperaldosteronism vs. bilateral aldosterone producing adenoma
- Differential Diagnosis of Adrenal Mass Using Imaging Modality: Special Emphasis on F-18 Fluoro-2-Deoxy-D-Glucose Positron Emission Tomography/Computed Tomography
- Primary Aldosteronism Due to Aldosterone Producing Adenama in the Presence of Contralateral Nonfunctioning Adenama
- 18F-FDG PET/CT and Sonographic Findings of Thyroid Incidentalomas
- Imaging of F-18 FDG PET/CT and follow up of bilateral invasive adrenal diffuse large B cell lymphoma mimicking adrenocortical carcinoma