J Korean Med Sci.
2008 Jun;23(3):502-508. 10.3346/jkms.2008.23.3.502.
The Effect of In Vivo Grown Corneal Epithelium Transplantation on Persistent Epithelial Defects with Limbal Stem Cell Deficiency
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Yongsan Hospital Chung-Ang University, Seoul, Korea. jck50ey@kornet.net
- 2Department of Pathology, College of Medicine, Yongsan Hospital Chung-Ang University, Seoul, Korea.
- KMID: 1786891
- DOI: http://doi.org/10.3346/jkms.2008.23.3.502
Abstract
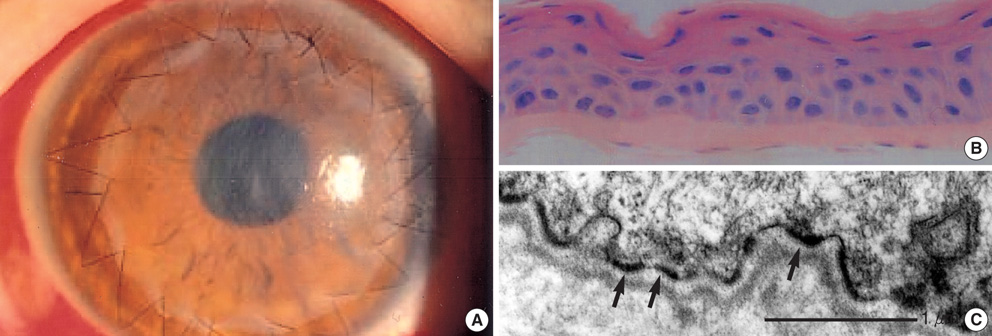
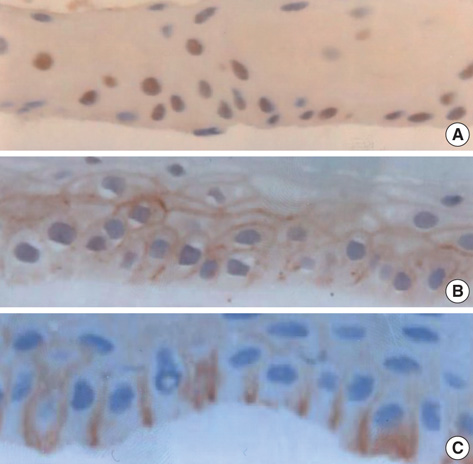
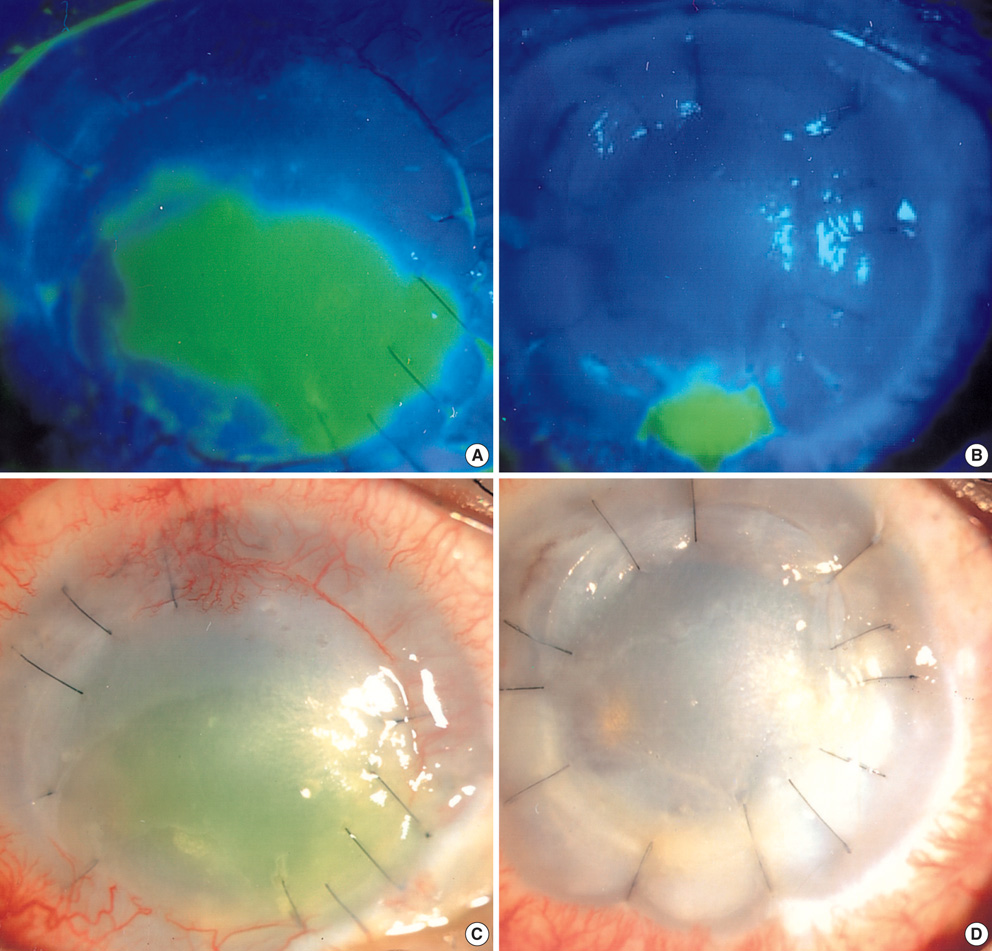
- We report our experience with corneal epithelium, grown in vivo, transplantation in three patients with persistent epithelial defect (PED). The three patients had ocular surface disease unresponsive to standard treatments and were therefore chosen for transplantation. They underwent transplantation of epithelial sheets, grown in vivo, to the most affected eye. In vivo cultivation was carried out in the cornea of a living related donor. After epithelialization was completed, the epithelium grown on an amniotic membrane was harvested gently; it was then transplanted into the patient's eye after debridement of fibrovascular tissue. The cultivated epithelium was completely epithelialized by 2 weeks; it was well-differentiated with well-formed hemidesmosome. On immunohistochemical staining, p63, connexin 43, and Integrin beta4 were expressed in the cells on the epithelial sheet. The PED was covered completely and maintained for 4 weeks in all cases. However, corneal erosion recurred after 5 weeks in two cases. This novel technique demonstrates the corneal epithelial cells can be expanded in vivo successfully on denuded amniotic membrane of a healthy cornea and harvested safely. A corneal epithelial sheet, grown in vivo, can be transplanted to treat eye with a severe ocular surface disease, such as total limbal deficiency.
Keyword
MeSH Terms
-
Adult
Cell Culture Techniques
Cells, Cultured
Corneal Diseases/etiology/pathology/*surgery
Corneal Transplantation/*methods
Epithelial Cells/cytology/*transplantation
Epithelium, Corneal/cytology/*transplantation
Eye Burns/complications
Humans
Limbus Corneae/*pathology
Male
Middle Aged
Stem Cells/*pathology
Stevens-Johnson Syndrome/complications
Figure
Reference
-
1. Shapiro MS, Friend J, Thoft RA. Corneal re-epithelialization from the conjunctiva. Invest Ophthalmol Vis Sci. 1981. 21:135–142.2. Thoft RA. Keratoepithelioplasty. AM J Ophthalmol. 1984. 97:1–6.
Article3. Kenyon KR, Tseng SC. Limbal autograft transplantation for ocular surface disorders. Ophthalmology. 1989. 96:709–722.
Article4. Kinoshita S, Manabe R. Brightbill FS, editor. Chemical burns. Corneal surgery, technique, and tissue. 1993. St. Louis, USA: Mosby;309–316.5. Tsai RJ, Tseng SC. Human allograft limbal transplantation for corneal surface reconstruction. Cornea. 1994. 13:389–400.
Article6. Pellegrini G, Traverso CE, Franzi AT, Zingirian M, Cancedda R, De Luca M. Long-term restoration of damaged corneal surfaces with autologous cultivated corneal epithelium. Lancet. 1997. 349:990–993.
Article7. Tsai RJ, Li LM, Chen JK. Reconstruction of damaged corneas by transplantation of autologous limbal epithelial cells. N Engl J Med. 2000. 343:86–93.
Article8. Schwab IR, Reyes M, Isseroff RR. Successful transplantation of bioengineered tissue replacements in patients with ocular surface disease. Cornea. 2000. 19:421–426.
Article9. Ha HS, Song KY, Kim JC. Ultrastructural analysis of in vivo expanded corneal epithelium on amniotic membrane. J Korean Med Sci. 2006. 21:544–549.
Article10. Tisdale AS, Spurr-Michaud SJ, Rodrigues M, Hackett J, Krachmer J, Gipson IK. Development of anchoring structures of the epithelium in rabbit and human fetal corneas. Invest Ophthalmol Vis Sci. 1988. 29:727–736.11. Kinoshita S, Koizumi N, Sotozono C, Yamada J, Nakamura T, Inatomi T. Concept and clincal application of cultivated epithelial transplantation for ocular surface disorders. Ocul Surf. 2004. 2:21–33.12. Rama P, Bonini S, Lambiase A, Golisano O, Paterna P, De Luca M, Pellegrini G. Autologous fibrin-cultured limbal stem cells permanently restore the corneal surface of patients with total limbal stem cell deficiency. Transplantation. 2001. 72:1478–1485.13. Koizumi N, Inatomi T, Suzuki T, Sotozono C, Kinoshita S. Cultivated corneal epithelial stem cell transplantation in ocular surface disorders. Ophthalmology. 2001. 108:1569–1574.14. Koizumi N, Inatomi T, Suzuki T, Sotozono C, Kinoshita S. Cultivated corneal epithelial transplantation for ocular surface reconstruction in acute phase Stevens-Johnson syndrome. Arch Ophthalmol. 2001. 119:298–300.15. Böhringer D, Spierings E, Enczmann J, Böhringer S, Sundmacher R, Goulmy E, Reinhard T. Matching of the minor histocompatibility antigen HLA-A1/H-Y may improve prognosis in corneal transplantation. Transplantation. 2006. 82:1037–1041.
Article16. Reinhard T, Böhringer D, Enczmann J, Kögler G, Mayweg S, Wernet P, Sundmacher R. Improvement of graft prognosis in penetrating normal-risk keratoplasty by HLA class I and II matching. Eye. 2004. 18:269–277.
Article17. Treseler PA, Foulks GN, Sanfilippo F. Expression of ABO blood group, hematopoietic, and other cell-specific antigens by cells in the human cornea. Cornea. 1985-86. 4:157–168.
Article18. Dua HS, Chan J, Gomes JA, Azuara-Blanco A. Adverse effect of blood group ABO mismatching on corneal epithelial cells. Lancet. 1998. 352:1677–1678.
Article19. Tisdale AS, Spurr-Michaud SJ, Rodriques M, Hackett J, Krachmer J, Gipson IK. Development of the anchoring structures of the epithelium in rabbit and human fetal cornea. Invest Ophthalmol Vis Sci. 1988. 29:727–736.20. Kim JC, Tseng SC. Transplantation of preserved human amniotic membrane for surface reconstruction in severely damaged rabbit corneas. Cornea. 1995. 14:473–484.
Article21. Koizumi N, Inatomi T, Quantock AJ, Fullwood NJ, Dota A, Kinoshita S. Amniotic membrane as a substrate for cultivating limbal corneal epithelial cells for autologous transplantation in rabbits. Cornea. 2000. 19:65–71.
Article22. Schwab IR, Reyes M, Isseroff RR. Successful transplantation of bioengineered tissue replacements in patients with ocular surface disease. Cornea. 2000. 19:421–426.
Article23. Koizumi N, Fullwood NJ, Bairaktaris G, Inatomi T, Kinoshita S, Quantock AJ. Cultivation of corneal epithelial cells on intact and denuded human amniotic membrane. Invest Ophthalmol Vis Sci. 2000. 41:2506–2513.24. Meller D, Pires RT, Tseng SC. Ex vivo preservation and expansion of human limbal epithelial stem cells on amniotic membrane cultures. Br J Ophthalmol. 2002. 86:463–471.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transplantation of in vivo Cultivated Limbal Corneal Epithelial Cells with Total Limbal Stem Cell Deficiency
- New Strategy of Ocular Surface Disease: Ocular Surface Reconstruction Using Amniotic Membrane and Limbal Stem Cell Transplantation
- Long-term Outcome of Limbal Epithelial Cells Cultivated in Vivo on Amniotic Membrane Transplantation
- Stepwise surgical approach for in vivo expansion of epithelial stem cells to treating severe acute chemical burns with total limbal deficiency
- Combined Surgery of the Penetrating Keratoplasty and the Limbal Cell Transplantation