J Korean Med Sci.
2008 Aug;23(4):740-743. 10.3346/jkms.2008.23.4.740.
Hypofractionated High-Dose Intensity-Modulated Radiotherapy (60 Gy at 2.5 Gy per Fraction) for Recurrent Renal Cell Carcinoma: A Case Report
- Affiliations
-
- 1Department of Radiation Oncology, Yonsei Cancer Center, Yonsei University Health System, Seoul, Korea. jjhmd@yuhs.ac
- 2Department of Urology, Urological Science Institute, Yonsei University Health System, Seoul, Korea.
- 3Division of Medical Oncology, Department of Internal Medicine, Yonsei University Health System, Seoul, Korea.
- 4Department of Pathology, Yonsei University Health System, Seoul, Korea.
- KMID: 1785842
- DOI: http://doi.org/10.3346/jkms.2008.23.4.740
Abstract
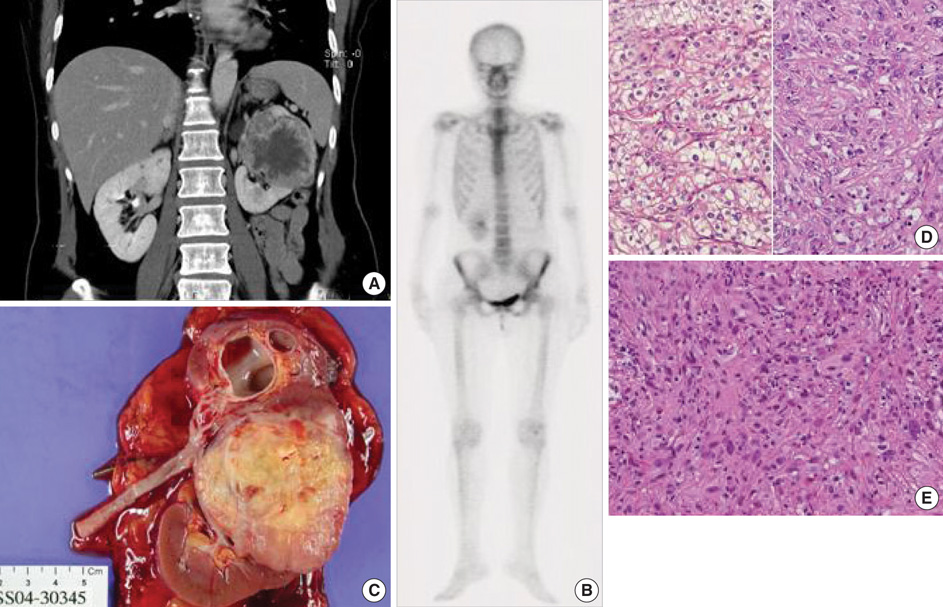
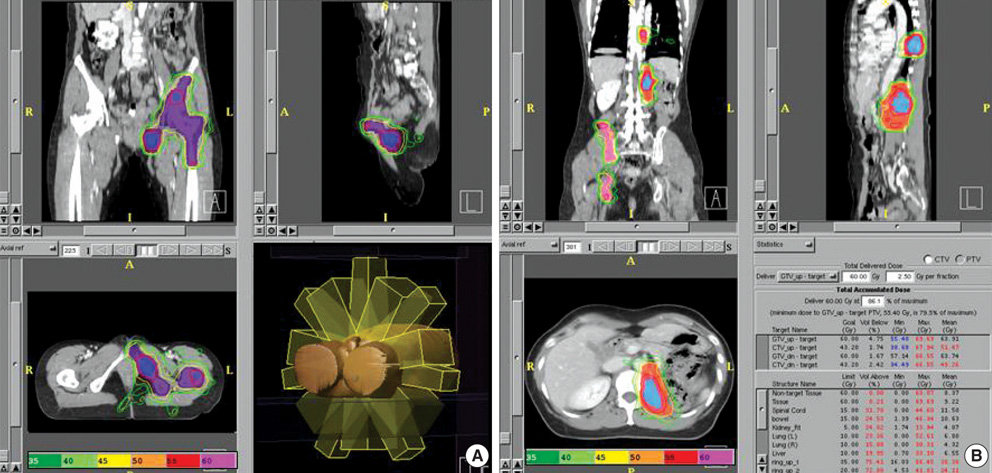
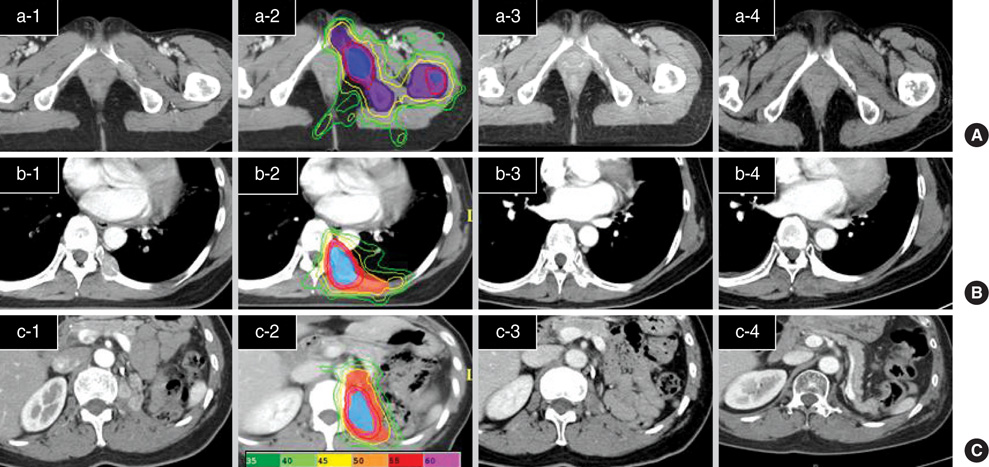
- A patient with renal cell carcinoma (RCC) developed synchronous bone metastasis with metachronous relapses to the bone and renal fossa. The primary lesion was initially removed surgically, and the metastatic bone lesions and locally recurrent tumours were treated by a high-fractional dose and high-total-dose intensitymodulated radiotherapy (IMRT, 60 Gy at 2.5 Gy per fraction) without significant side effects. All the grossly relapsed tumors underwent complete remission (CR) within a short time after IMRT. To date, CR has been maintained for more than two years. This case study reports the successful treatment of radioresistant RCC using a new scheme that involves a fractionation regimen with a high precision radiotherapy.
MeSH Terms
Figure
Reference
-
1. DiBiase SJ, Valicenti RK, Schultz D, Xie Y, Gomella LG, Corn BW. Palliative irradiation for focally symptomatic metastatic renal cell carcinoma: support for dose escalation based on a biological model. J Urol. 1997. 158:746–749.
Article2. Wronski M, Maor MH, Davis BJ, Sawaya R, Levin VA. External radiation of brain metastases from renal carcinoma: a retrospective study of 119 patients from the M. D. Anderson Cancer Center. Int J Radiat Oncol Biol Phys. 1997. 37:753–759.3. Fertil B, Malaise EP. Intrinsic radiosensitivity of human cell lines is correlated with radioresponsiveness of human tumors: analysis of 101 published survival curves. Int J Radiat Oncol Biol Phys. 1985. 11:1699–1707.
Article4. Sheehan JP, Sun MH, Kondziolka D, Flickinger J, Lunsford LD. Radiosurgery in patients with renal cell carcinoma metastasis to the brain: long-term outcomes and prognostic factors influencing survival and local tumor control. J Neurosurg. 2003. 98:342–349.
Article5. Gogus C, Baltaci S, Beduk Y, Sahinli S, Kupeli S, Gogus O. Isolated local recurrence of renal cell carcinoma after radical nephrectomy: experience with 10 cases. Urology. 2003. 61:926–929.
Article6. Itano NB, Blute ML, Spotts B, Zincke H. Outcome of isolated renal cell carcinoma fossa recurrence after nephrectomy. J Urol. 2000. 164:322–325.
Article7. Schrodter S, Hakenberg OW, Manseck A, Leike S, Wirth MP. Outcome of surgical treatment of isolated local recurrence after radical nephrectomy for renal cell carcinoma. J Urol. 2002. 167:1630–1633.8. Master VA, Gottschalk AR, Kane C, Carroll PR. Management of isolated renal fossa recurrence following radical nephrectomy. J Urol. 2005. 174:473–477.
Article9. Tanguay S, Pisters LL, Lawrence DD, Dinney CP. Therapy of locally recurrent renal cell carcinoma after nephrectomy. J Urol. 1996. 155:26–29.
Article10. Figlin RA, Abi-Aad AS, Belldegrun A, deKernion JB. The role of interferon and interleukin-2 in the immunotherapeutic approach to renal cell carcinoma. Semin Oncol. 1991. 18(5 Supple 7):102–107.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hypofractionated radiotherapy for early glottic cancer: a retrospective interim analysis of a single institution
- Hypofractionated intensity-modulated radiotherapy in patients with localized prostate cancer: a preliminary study
- Treatment Outcomes of Helical Intensity-Modulated Radiotherapy for Unresectable Hepatocellular Carcinoma
- Evaluation of the Treatment Response after Hypofractionated Radiotherapy in Patients with Advanced Head and Neck Cancers
- Feasibility and Outcomes of Hypofractionated Simultaneous Integrated Boost-Intensity Modulated Radiotherapy for Malignant Gliomas: A Preliminary Report