J Korean Med Sci.
2008 Aug;23(4):731-733. 10.3346/jkms.2008.23.4.731.
Subconjuctival Loa loa with Calabar Swelling
- Affiliations
-
- 1Department of Ophthalmology, Hanyang University Guri Hospital, Guri, Korea.
- 2Department of Parasitology, Hanyang University College of Medicine, Seoul, Korea. jsryu@hanyang.ac.kr
- KMID: 1785839
- DOI: http://doi.org/10.3346/jkms.2008.23.4.731
Abstract
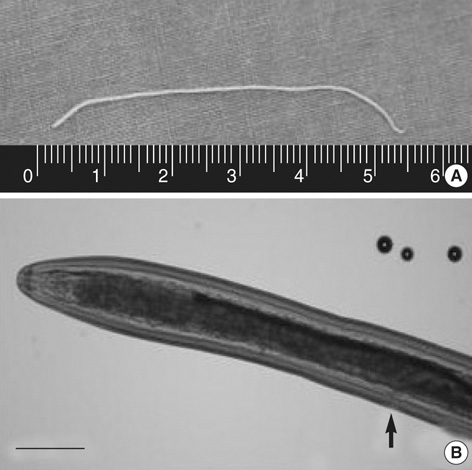
- Loa loa is unique among the human filariae in that adult worms are occasionally visible during subconjuntival migration. A 29-yr-old African female student, living in Korea for the past 5 yr without ever visiting her home country, presented with acute eyelid swelling and a sensation of motion on the left eyeball. Her symptoms started one day earlier and became worse over time. Examination revealed a threadlike worm beneath the left upper bulbar conjunctiva with mild eyelid swelling as well as painless swelling of the right forearm. Upon exposure to slit-lamp illumination, a sudden movement of the worm toward the fornix was noted. After surgical extraction, parasitologic analysis confirmed the worm to be a female adult Loa loa with the vulva at the extreme anterior end. On blood smear, the microfilariae had characteristic features of Loa loa, including sheath and body nuclei up to the tip of the tail. The patient also showed eosinophilia (37%) measuring 4,100/microliter. She took ivermectin (200 microgram/kg) as a single dose and suffered from a mild fever and chills for one day. This patient, to the best of our knowledge, is the first case of subconjunctival loiasis with Calabar swelling in Korea.
Keyword
MeSH Terms
Figure
Reference
-
1. Klion AD, Massougbodji A, Sadeler BC, Ottesen EA, Nutman TB. Loiasis in endemic and nonendemic populations: immunologically mediated differences in clinical presentation. J Infect Dis. 1991. 163:1318–1325.
Article2. Min DY, Soh CT, Yoon JW. A case of Calabar swelling suspected as loiasis. Korean J Parasitol. 1987. 25:185–187.
Article3. Chun YS, Chun SI, Im KI, Moon TK, Lee MG. A case of loiasis. Yonsei Med J. 1998. 39:184–188.
Article4. Boussinesq M, Gardon J. Prevalences of Loa loa microfilaraemia throughout the area endemic for the infection. Ann Trop Med Parasitol. 1997. 91:573–589.5. Churchill DR, Morris C, Fakoya A, Wright SG, Davidson RN. Clinical and laboratory features of patients with loiasis (Loa loa filariasis) in the U.K. J Infect. 1996. 33:103–109.
Article6. Thomas J, Chastel C, Forcain L. Latence clinique et parasitaire dans les filarioses a Loa loa et a Onchocerca volvulus. Bull Soc Pathol Exot Filiales. 1970. 63:90–94.7. Toure FS, Deloron P, Egwang TG, Wahl G. Relation entre intensite de la transmission de la filaire Loa loa et prevalence des infections. Med Trop (Mars). 1999. 59:249–252.8. Pion SD, Demanou M, Oudin B, Boussinesq M. Loiasis: the individual factors associated with the presence of microfilaraemia. Ann Trop Med Parasitol. 2005. 99:491–500.
Article9. Beaver PC, Jung RC, Cupp EW. Loa loa. Clinical Parasitology. 1984. Washington: Lea & Febiger;377–380.10. Toure FS, Mavoungou E, Deloron P, Egwang TG. Analyse comparative de deux methods diagnostiques de la loase humaine: serologie IgG4 et PCR niche. Bull Soc Pathol Exot. 1999. 92:167–170.11. Klion AD, Vijaykumar A, Oei T, Martin B, Nutman TB. Serum immunoglobulin G4 antibodies to the recombinant antigen, Ll-SXP-1, are highly specific for Loa loa infection. J Infect Dis. 2003. 187:128–133.12. Toure FS, Egwang TG, Wahl G, Millet P, Bain O, Georges AJ. Species-specific sequence in the repeat 3 region of the gene encoding a putative Loa loa allergen: a diagnostic for occult loiasis. Am J Trop Med Hyg. 1997. 56:57–60.13. Toure FS, Kassambara L, Williams T, Millet P, Bain O, Georges AJ, Egwang TG. Human occult loiasis: improvement in diagnostic sensitivity by the use of a nested polymerase chain reaction. Am J Trop Med Hyg. 1998. 59:144–149.14. Boussinesq M. Loiasis. Ann Trop Med Parasitol. 2006. 8:715–731.
Article15. John DT, Petri WA Jr. Examination of blood, other body fluids and tissues, sputum, and urine. Markell and Voge's Medical Parasitology. 2006. St. Louis: Saunders Elsevier;422.16. Gardon J, Gardon-Wendel N, Demanga-Ngangue , Kamgno J, Chippaux JP, Boussinesq M. Serious reactions after mass treatment of onchocerciasis with ivermectin in an area endemic for Loa loa infection. Lancet. 1997. 350:18–22.
Article17. Boussinesq M, Gardon J, Gardon-Wendel N, Chippaux JP. Clinical picture, epidemiology, and outcome of Loa-associated adverse events related to mass ivermectin treatment of onchocerciasis in Cameroon. Filaria J. 2003. 2:Suppl 1. S4.