J Korean Med Sci.
2008 Aug;23(4):579-585. 10.3346/jkms.2008.23.4.579.
The Usefulness of Percutaneous Transhepatic Cholangioscopy for Identifying Malignancies in Distal Commom Bile Duct Strictures
- Affiliations
-
- 1Department of Internal Medicine, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. sklee@amc.seoul.kr
- 2Department of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- KMID: 1785813
- DOI: http://doi.org/10.3346/jkms.2008.23.4.579
Abstract
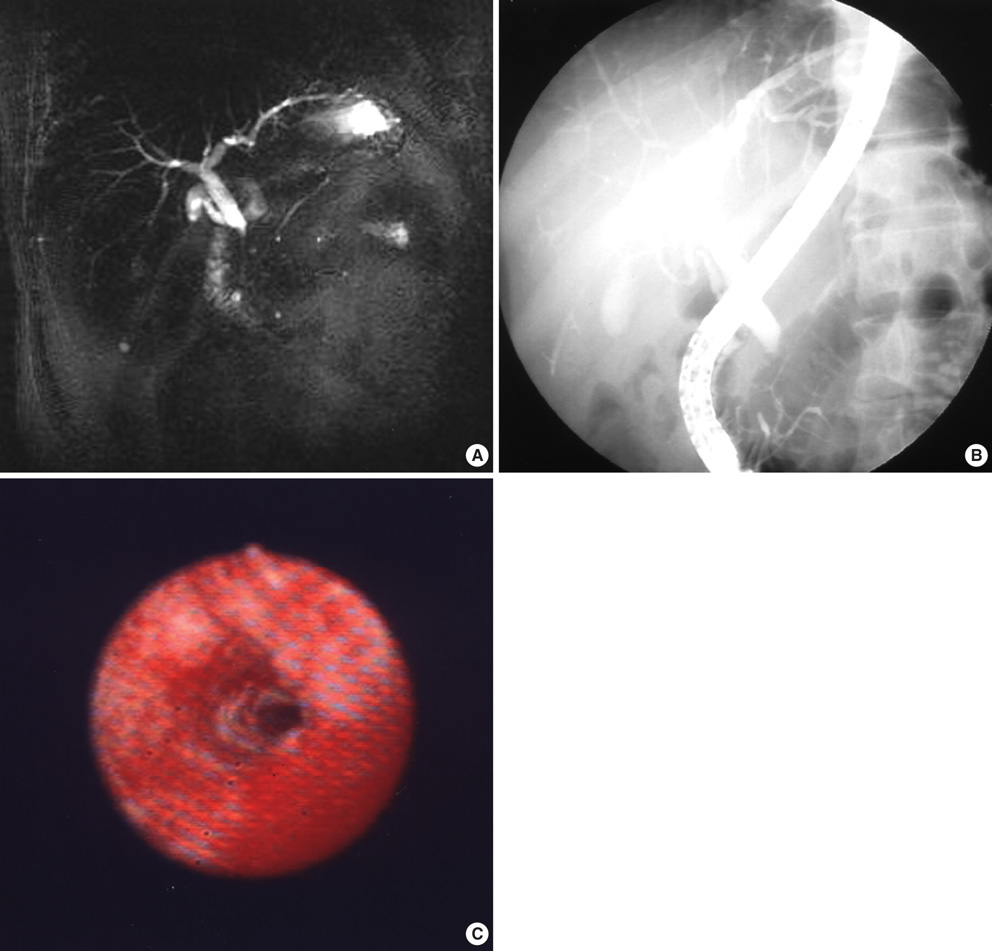
- The diagnostic accuracy of percutaneous transhepatic cholangioscopy (PTCS) was compared to that of three radiologic modalities in distal common bile duct (CBD) strictures for the evaluation of clinical application. Ninety-five patients who underwent PTCS for the evaluation of distal CBD strictures (35 malignant and 60 benign) whose masses were not obvious from radiologic imagings were included. Confirmative diagnosis could not be reached by endoscopic retrograde cholangiopancreatography (ERCP) or radiologic findings in all cases. Specific findings on the computed tomography (CT), magnetic resonance cholangiopancreatography (MRCP) and direct cholangiography were analyzed among 68 (25 malignant and 43 benign) out of the 95 patients in order to determine the sensitivity and specificity of three radiologic studies for the diagnosis of malignant distal CBD strictures, and to compare those results with those by a combination of PTCS-guided biopsy and tumor vessel observation on cholangioscopy. The sensitivity/specificity of CT, MRCP and direct cholangiography including ERCP in diagnosing malignant distal CBD strictures were 42.9%/65.8%, 53.3%/58.3%, and 70.8%/47.6% respectively, while it was 96%/100% for the combination of PTCS-guided biopsy and tumor vessel. PTCS is a useful method for differential diagnosis of distal CBD strictures, particularly when it is difficult to distinguish benign from malignant strictures by radiologic studies and when peroral approach is not feasible.
Keyword
MeSH Terms
Figure
Reference
-
1. Nimura Y. Staging of biliary carcinoma: cholangiography and cholangioscopy. Endoscopy. 1993. 23:76–80.
Article2. Van Steenbergen W, Van Aken L, Van Beckevoort D, Stockx L, Fevery J. Percutaneous transhepatic cholangioscopy for diagnosis and therapy of biliary diease in older patients. J Am Geriatr Soc. 1996. 44:1384–1387.3. Yeh YH, Huang MH, Yang JC, Mo LR, Lin J, Yueh SK. Percutaneous transhepatic cholangioscopy and lithotripsy in the treatment of intrahepatic stones: a study with 5 year follow-up. Gastrointest Endosc. 1995. 42:13–18.
Article4. Hawes RH. Diagnostic and therapeutic uses of ERCP in pancreatic and biliary tract malignancies. Gastrointest Endosc. 2002. 56:S201–S205.
Article5. Nimura Y, Kamiya J, Hayakawa N, Shionoya S. Cholangioscopic differentiation of biliary strictures and polyps. Endoscopy. 1989. 21:Suppl 1. 351–356.
Article6. Neuhaus H. Cholangioscopy. Endoscopy. 1992. 24:125–132.
Article7. Nakajima M, Akasaka Y, Fukumoto K, Mitsuyoshi Y, Kawai K. Peroral cholangiopancreatoscopy (PCPS) under duodenoscopic guidance. Am J Gastroenterol. 1976. 66:241–247.8. Urakami Y, Seifert E, Butke H. Peroral direct cholangioscopy (PDCS) using routine straight-view endoscope: first report. Endoscopy. 1977. 9:27–30.
Article9. Frimberger E, Vente T, Wagenpfeil S, Gerein P, Born P, Fritz N, Allescher HD, Ott R, Weigert N, Classen M, Rosch T. A new system for rapid large-caliber percutaneous transhepatic drainage in patients with obstructive jaundice: a prospective randomized trial. Endoscopy. 2001. 33:201–209.
Article10. Kim MH. Percutaneous transhepatic cholangioscopic examination: a necessity for the biliary endoscopist. Gastrointest Endosc. 2001. 53:695–697.
Article11. Classen M, Neuhaus H. Diagnostic and therapeutic peroral and percutaneous cholangioscopy. J Gastroenterol. 1994. 29:Suppl 7. 143–147.12. Kim HJ, Kim MH, Lee SK, Yoo KS, Seo DW, Min YI. Tumor vessel: a valuable cholangioscopic clue of malignant biliary stricture. Gastrointest Endosc. 2000. 52:635–638.
Article13. Hwang MH, Tsai CC, Chou CY, Mo LR, Yang CT, Lin RC, Yueh SK. Percutaneous cholangiofiberscopic endoluminal forceps biopsy of intrabile duct diseases. Hepatogastroenterology. 1998. 45:2073–2078.14. Rosch T, Hofrichter K, Frimberger E, Meining A, Born P, Weigert N, Allescher HD, Classen M, Barbur M, Schenck U, Werner M. ERCP or EUS for tissue diagnosis of biliary strictures? A prospective comparative study. Gastrointest Endosc. 2004. 60:390–396.15. Pugliese V, Conio M, Nicolo G, Saccomanno S, Gatteschi B. Endoscopic retrograde forceps biopsy and brush cytology of biliary stricture: a prospective study. Gastrointest Endosc. 1995. 42:520–526.16. Sato M, Inoue S, Ogawa , Ohashi S, Maetani I, Igarashi Y, Sakai Y. Limitations of percutaneous transhepatic cholangioscopy for diagnosis of the intramural extension of bile duct carcinoma. Endoscopy. 1998. 30:281–288.17. Yamase H, Nimura Y, Hayakawa N. Differential diagnosis on stenosis of ductal bile duct by percutaneous transhepatic cholangioscopy (in Japanese). Gastroenterol Endosc. 1988. 30:175–182.18. Bhutani MS, Hawes RH, Baron PL, Sanders-Cliette A, Van Velse A, Osborne JF, Osborne JF, Hoffman BJ. Endoscopic ultrasound (EUS) guided fine needle aspiration of malignant pancreatic lesions. Endoscopy. 1997. 29:854–858.19. Binmoeller KF, Thul R, Rathod V, Henke P, Brand B, Jabusch HC, Soehendra N. Endoscopic ultrasound-guided, 18-gauge, fine-needle aspiration biopsy of the pancreas using a 2.8 mm channel convex echoendoscope. Gastrointest Endosc. 1998. 47:121–127.20. Chang KJ, Katz KD, Durbin TE, Erickson RA, Butler JA, Lin F, Wuerker RB. Endoscopic ultrasound-guided fine-needle aspiration. Gastrointest Endosc. 1994. 40:694–699.
Article21. Fritscher-Ravens A, Sriram P, Krause C, Atay Z, Jaeckle S, Thonke F, Brand B, Bohnacker S, Soehendra N. Detection of pancreatic metastases by EUS-guided fine-needle aspiration. Gastrointest Endosc. 2001. 53:65–70.
Article22. Giovannini M, Seitz JF, Monges G, Rabbia I, Perrier H. Fine-needle aspiration biopsy guided by endoscopic ultrasonography. Results in 141 patients. Endoscopy. 1995. 27:171–177.23. Gress F, Gottlieb K, Sherman S, Lehman G. Endoscopic ultrasonography-guided fine-needle aspiration biopsy of suspected pancreatic cancer. Ann Intern Med. 2001. 134:459–464.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Transhepatic Cholangioscopy: Does Its Role Still Exist?
- Usefulness of Cholangioscopy in Patients with Focal Stricture of the Intrahepatic Duct Unrelated to Intrahepatic Stones
- Hepatocellular Carcinoma with Obstructive Jaundice Confirmed by Percutaneous Transhepatic Cholangioscopy (PTCS) and Peroral Cholangioscopy (POCS)
- Two Cases of Percutaneous Transhepatic Choledochoscopy Treatment of Intrahepatic Duct Stones that Occurred after Living Donor Liver Transplantation
- Percutaneous Transhepatic Therapy Using Cholangioscopy in Patients with Benign Bilio-Enteric Anastomotic Strictures