J Korean Med Sci.
2004 Feb;19(1):87-94. 10.3346/jkms.2004.19.1.87.
A Prospective Randomized Study on Two Dose Fractionation Regimens of High-Dose-Rate Brachytherapy for Carcinoma of the Uterine Cervix: Comparison of Efficacies and Toxicities Between Two Regimens
- Affiliations
-
- 1Department of Radiation Oncology, Chonnam National University Medical School, Gwangju, Korea. ahnsja@chonnam.ac.kr
- KMID: 1785700
- DOI: http://doi.org/10.3346/jkms.2004.19.1.87
Abstract
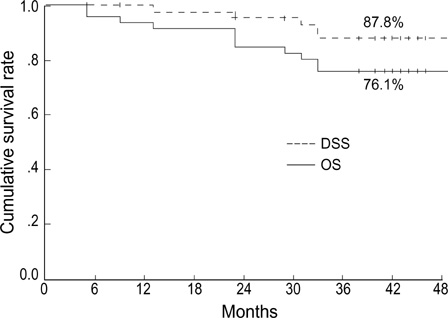
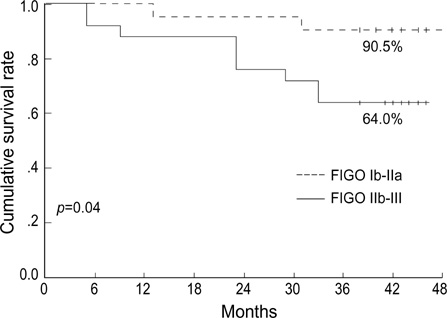
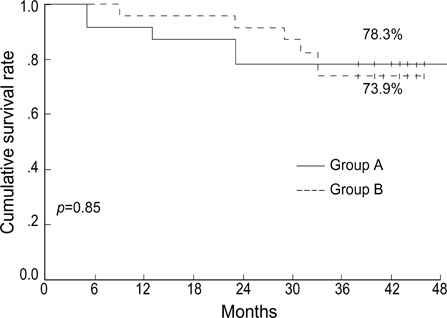
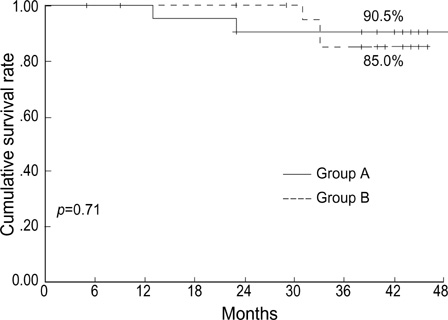
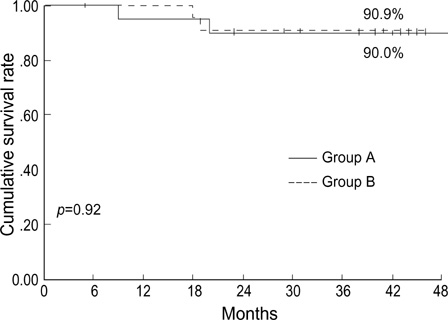
- To evaluate the toxicities and efficacies of two fractionation regimens of high-doserate brachytherapy in uterine cervical cancer, patients were stratified by stage Ib- IIa versus IIb-IVa, and randomly assigned to receive 3 Gy fractions (group A) or 5 Gy fractions (group B). External radiotherapy was performed using a 10 MV radiography with a daily 1.8 Gy up to 30.6 Gy to the whole pelvis, and then with a midline shield up to 45.0 Gy. Brachytherapy was performed with 3 Gy x 10 times or 5 Gy x5 times, and this was followed by booster brachytherapy of a smaller fraction to the residual tumor. Between August 1999 to July 2000, 46 patients were eligible. Median follow-up period was 42 months (5-49). The range of age was 37-83 yr (median, 58). The three-year disease-specific survival rates of group A (n=23) and B (n=23) were 90.5%, 84.9%, respectively (p=0.64). The three-year pelvic control rates of group A and B were 90.0% and 90.9%, respectively (p=0.92). The incidences of late complications of the rectum or bladder of grade 2 or greater in groups A and B were 23.8% and 9.1%, respectively (p=0.24). Our study showed that the results of two regimens were comparable. Fractionation regimen using 5 Gy fractions seems to be safe and effective, and offers shorter treatment duration.
MeSH Terms
Figure
Reference
-
1. Ministry of Health and Welfare. Annual report of the Korea Central Cancer Registry Program: Based on registered data from 134 hospitals, January-December, 2001. 2002. Korea:2. Fu KK, Phillips TL. High-dose-rate versus low-dose-rate intracavitary brachytherapy for carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 1990. 19:791–796.
Article3. Patel FD, Sharma SC, Negi PS, Ghoshal S, Gupta BD. Low dose rate vs. high dose rate brachytherapy in the treatment of carcinoma of the uterine cervix: a clinical trial. Int J Radiat Oncol Biol Phys. 1994. 28:335–341.
Article4. Huh SJ. Current status of high dose rate brachytherapy in cervical cancer in Korea and optimal treatment schedule. J Korean Soc Ther Radiol Oncol. 1998. 16:357–366.5. Nag S, Erickson B, Thomadsen B, Orton C, Demanes JD, Petereit D. The American Brachytherapy Society recommendations for high-dose-rate brachytherapy for carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 2000. 48:201–211.
Article6. Lee SW, Suh CO, Chung EJ, Kim GE. Dose optimization of fractionated external radiation and high-dose-rate intracavitary brachytherapy for FIGO stage IB uterine cervical carcinoma. Int J Radiat Oncol Biol Phys. 2002. 52:1338–1344.
Article7. Sood BM, Gorla G, Gupta S, Garg M, Deore S, Runowicz CD, Fields AL, Goldberg GL, Anderson PS, Vikram B. Two fractions of high-dose-rate brachytherapy in the management of cervix cancer: clinical experience with and without chemotherapy. Int J Radiat Oncol Biol Phys. 2002. 53:702–706.
Article8. Ferrigno R, dos Santos Novaes PE, Pellizzon AC, Maia MA, Fogarolli RC, Gentil AC, Salvajoli JV. High-dose-rate brachytherapy in the treatment of uterine cervix cancer. Analysis of dose effectiveness and late complications. Int J Radiat Oncol Biol Phys. 2001. 50:1123–1135.
Article9. Le Pechoux C, Akine Y, Sumi M, Tokuuye K, Ikeda H, Yajima M, Yamada T, Tanemura K, Tsunematsu R, Ohmi K. High dose rate brachytherapy for carcinoma of the uterine cervix: comparison of two different fractionation regimens. Int J Radiat Oncol Biol Phys. 1995. 31:735–741.10. Wong FC, Tung SY, Leung TW, Sze WK, Wong VY, Lui CM, Yuen KK, O SK. Treatment results of high-dose-rate remote afterloading brachytherapy for cervical cancer and retrospective comparison of two regimens. Int J Radiat Oncol Biol Phys. 2003. 55:1254–1264.
Article11. Chatani M, Matayoshi Y, Masaki N, Teshima T, Inoue T. A prospective randomized study concerning the point A dose in high-dose rate intracavitary therapy for carcinoma of the uterine cervix. The final results. Strahlenther Onkol. 1994. 170:636–642.12. Dale RG. The application of the linear-quadratic dose-effect equation to fractionated and protracted radiotherapy. Br J Radiol. 1985. 58:515–528.
Article13. Fowler JF. The linear-quadratic formula and progress in fractionated radiotherapy. Br J Radiol. 1989. 62:679–694.
Article14. ICRU Report 38. Dose and volume specification for reporting intracavitary therapy in gynecology. 1985. International commission on radiation units and measurements;1–20.15. Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995. 31:1341–1346.
Article16. Stitt JA, Fowler JF, Thomadsen BR, Buchler DA, Paliwal BP, Kinsella TJ. High dose rate intracavitary brachytherapy for carcinoma of the cervix: the Madison system: I. Clinical and radiobiological considerations. Int J Radiat Oncol Biol Phys. 1992. 24:335–348.
Article17. Orton CG. High-dose-rate brachytherapy may be radiobiologically superior to low-dose rate due to slow repair of late-responding normal tissue cells. Int J Radiat Oncol Biol Phys. 2001. 49:183–189.
Article18. Nag S, Orton C, Young D, Erickson B. The American brachytherapy society survey of brachytherapy practice for carcinoma of the cervix in the United States. Gynecol Oncol. 1999. 73:111–118.
Article19. Petereit DG, Pearcey R. Literature analysis of high dose rate brachytherapy fractionation schedules in the treatment of cervical cancer: is there an optimal fractionation schedule? Int J Radiat Oncol Biol Phys. 1999. 43:359–366.
Article20. Nag S, Gupta N. A simple method of obtaining equivalent doses for use in HDR brachytherapy. Int J Radiat Oncol Biol Phys. 2000. 46:507–513.
Article21. Clark BG, Souhami L, Roman TN, Chappell R, Evans MD, Fowler JF. The prediction of late rectal complications in patients treated with high dose-rate brachytherapy for carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 1997. 38:989–993.
Article22. Toita T, Kakinohana Y, Ogawa K, Adachi G, Moromizato H, Nagai Y, Maehama T, Sakumoto K, Kanazawa K, Murayama S. Combination external beam radiotherapy and high-dose-rate intracavitary brachytherapy for uterine cervical cancer: analysis of dose and fractionation schedule. Int J Radiat Oncol Biol Phys. 2003. 56:1344–1353.
Article23. Ogino I, Kitamura T, Okamoto N, Yamasita K, Aikawa Y, Okajima H, Matsubara S. Late rectal complication following high dose rate intracavitary brachytherapy in cancer of the cervix. Int J Radiat Oncol Biol Phys. 1995. 31:725–734.
Article24. Potter R, Van Limbergen E, Gerstner N, Wambersie A. Survey of the use of the ICRU 38 in recording and reporting cervical cancer brachytherapy. Radiother Oncol. 2001. 58:11–18.25. Kapp KS, Stuecklschweiger GF, Kapp DS, Poschauko J, Pickel H, Hackl A. Carcinoma of the cervix: analysis of complications after primary external beam radiation and Ir-192 HDR brachytherapy. Radiother Oncol. 1997. 42:143–153.
Article26. Van Lancker M, Storme G. Prediction of severe late complications in fractionated, high dose-rate brachytherapy in gynecological applications. Int J Radiat Oncol Biol Phys. 1991. 20:1125–1129.
Article27. Uno T, Itami J, Aruga M, Kotaka K, Fujimoto H, Sato T, Minoura S, Ito H. High dose rate brachytherapy for carcinoma of the cervix: risk factors for late rectal complications. Int J Radiat Oncol Biol Phys. 1998. 40:615–621.
Article28. Rose PG, Bundy BN, Watkins EB, Thigpen JT, Deppe G, Maiman MA, Clarke-Pearson DL, Insalaco S. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med. 1999. 340:1144–1153.
Article29. Whitney CW, Sause W, Bundy BN, Malfetano JH, Hannigan EV, Fowler WC Jr, Clarke-Pearson DL, Liao SY. Randomized comparison of fluorouracil plus cisplatin versus hydroxyurea as an adjunct to radiation therapy in stage IIB-IVA carcinoma of the cervix with negative para-aortic lymph nodes: a Gynecologic Oncology Group and Southwest Oncology Group study. J Clin Oncol. 1999. 17:1339–1348.
Article30. Morris M, Eifel PJ, Lu J, Grigsby PW, Levenback C, Stevens RE, Rotman M, Gershenson DM, Mutch DG. Pelvic radiation with concurrent chemotherapy compared with pelvic and para-aortic radiation for high-risk cervical cancer. N Engl J Med. 1999. 340:1137–1143.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status of High Dose Rate Brachytherapy in Cervical Cancer in Korea and Optimal Treatment Schedule
- Accuracy of Dose Estimation in High Dose Rate Intracavitary Radiotherapy of Carcinoma of the Uterine Cervix
- High-Dose-Rate Brachytherapy for Uterine Cervical Cancer : The Results of Different Fractionation Regimen
- Fractionated High-Dose-Rate Brachytherapy in the Management of Uterine Cervical Cancer
- Development of Source Template ICRT Dose Planning Software for Uterine Cervix Using the HDR: 192Ir