J Korean Acad Periodontol.
2009 Mar;39(1):27-36. 10.5051/jkape.2009.39.1.27.
Clinical and radiographic evaluation of implants with dual-microthread: 1-year study
- Affiliations
-
- 1Department of Periodontology, School of Dentistry, Pusan National University, Korea. heroine@pusan.ac.kr
- 2Department of Oral & Maxillofacial Surgery, School of Dentistry, Pusan National University, Korea.
- 3Department of Prosthodintics, School of Dentistry, Pusan National University, Korea.
- KMID: 1783513
- DOI: http://doi.org/10.5051/jkape.2009.39.1.27
Abstract
-
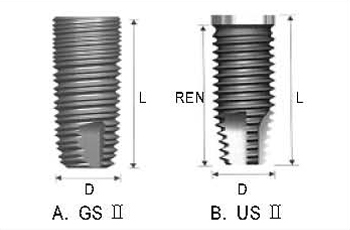
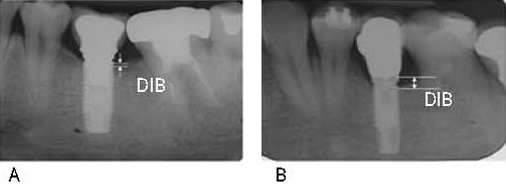
PURPOSE: The stability of periodontal condition and marginal bone level were important to achieve long-term success of dental implant treatment. The aim of this study was to evaluate periodontal conditions and marginal bone loss around 67 GSII(OSSTEM, Seoul, Korea) dental implants with dual-microthread at the neck portion, 1 year after prosthetic loading.
MATERIALS AND METHODS
Sixty-seven GS II dental implants in 27 patients(mean age; 47.4+/-4.0 years) who received implant treatments at Pusan National University Hospital, were included in this study. Thirteen US II(OSSTEM, Seoul, Korea) implants with smooth neck design were selected for the control group. Periodontal and radiographic evaluations were carried out at baseline, 6 months and 12 months after prosthetic loading.
RESULTS
In the GS II group, plaque index(PI), gingival index(GI) and probing depth(PD) increased as time passed. In the US II group, GI and PD increased. Although marginal bone level was lower in the US II group in all evaluation periods, the changes between the periods were not statistically significant(p>00.05). In each period, periodontal parameters were not statistically significant between groups.
CONCLUSION
One year after prosthetic loading, GS II and US II dental implants showed similar periodontal conditions and marginal bone response, and were within the criteria of success
MeSH Terms
Figure
Cited by 1 articles
-
Influence of microthread design on marginal cortical bone strain developement: A finite element analysis
Seung-Geun Chun, Jin-Hyun Cho, Kwang-Heon Jo
J Korean Acad Prosthodont. 2010;48(3):215-223. doi: 10.4047/jkap.2010.48.3.215.
Reference
-
1. Branemark PI, Adell R, Breine U, et al. Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand J Plast Reconstr Surg. 1969. 3:81–100.
Article2. Esposito M, Grusovin MG, Coulthard P, et al. A 5-year follow-up comparative analysis of the efficacy of various osseointegrated dental implant systems: A systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants. 2005. 20:557–568.3. Chang M, Wennstrom JL, Odman P, Andersson B. Implant supported single-tooth replacements compared to contralateral natural teeth. Crown and soft tissue dimensions. Clin Oral Implants Res. 1999. 10:185–194.
Article4. Hansson S. The implant neck: Smooth or provided with retention elements. A biomechanical approach. Clin Oral Implants Res. 1999. 10:394–405.
Article5. Abrahamsson I, Berglundh T. Tissue characteristics at microthreaded implants: An experimental study in dogs. Clin Implant Dent Relat Res. 2006. 8:107–113.
Article6. Palmer RM, Palmer PJ, Smith BJ. A 5-year prospective study of Astra single tooth implants. Clin Oral Implants Res. 2000. 11:179–182.
Article7. Lee DW, Choi YS, Park KH, et al. Effect of microthread on the maintenance of marginal bone level: A 3-year prospective study. Clin Oral Implants Res. 2007. 18:465–470.
Article8. Berglundh T, Persson L, Klinge B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol. 2002. 29:Suppl 3. 197–212. discussion 232-233.
Article9. Valderhaug J, Birkeland JM. Periodontal conditions in patients 5 years following insertion of fixed prostheses. Pocket depth and loss of attachment. J Oral Rehabil. 1976. 3:237–243.
Article10. Schroeder A, van der Zypen E, Stich H, Sutter F. The reactions of bone, connective tissue, and epithelium to endosteal implants with titanium-sprayed surfaces. J Maxillofac Surg. 1981. 9:15–25.
Article11. Cochran DL, Hermann JS, Schenk RK, et al. Biologic width around titanium implants. A histometric analysis of the implanto-gingival junction around unloaded and loaded nonsubmerged implants in the canine mandible. J Periodontol. 1997. 68:186–198.
Article12. Mombelli A, van Oosten MA, Schurch E Jr, Land NP. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol. 1987. 2:145–151.
Article13. Mombelli A, Lang NP. Clinical parameters for the evaluation of dental implants. Periodontol 2000. 1994. 4:81–86.
Article14. Astrand P, Engquist B, Dahlgren S, et al. Astra tech and branemark system implants: A prospective 5-year comparative study. results after one year. Clin Implant Dent Relat Res. 1999. 1:17–26.
Article15. Engquist B, Astrand P, Dahlgren S, et al. Marginal bone reaction to oral implants: A prospective comparative study of astra tech and branemark system implants. Clin Oral Implants Res. 2002. 13:30–37.16. Schou S, Holmstrup P, Hjorting-Hansen E, Lang NP. Plaque-induced marginal tissue reactions of osseointegrated oral implants: A review of the literature. Clin Oral Implants Res. 1992. 3:149–161.
Article17. Quirynen M, van Steenberghe D, Jacobs R, et al. The reliability of pocket probing around screw-type implants. Clin Oral Implants Res. 1991. 2:186–192.
Article18. Bengazi F, Wennstrom JL, Lekholm U. Recession of the soft tissue margin at oral implants. A 2-year longitudinal prospective study. Clin Oral Implants Res. 1996. 7:303–310.
Article19. Adell R, Lekholm U, Rockler B, et al. Marginal tissue reactions at osseointegrated titanium fixtures (I). A 3-year longitudinal prospective study. Int J Oral Maxillofac Surg. 1986. 15:39–52.20. Quirynen M, Naert I, van Steenberghe D. Fixture design and overload influence marginal bone loss and fixture success in the Branemark system. Clin Oral Implants Res. 1992. 3:104–111.
Article21. Engquist B, Nilson H, Astrand P. Single-tooth replacement by osseointegrated branemark implants. A retrospective study of 82 implants. Clin Oral Implants Res. 1995. 6:238–245.
Article22. Oh TJ, Yoon J, Misch CE, Wang HL. The causes of early implant bone loss: Myth or science? J Periodontol. 2002. 73:322–333.
Article23. Jung YC, Han CH, Lee KW. A 1-year radiographic evaluation of marginal bone around dental implants. Int J Oral Maxillofac Implants. 1996. 11:811–818.24. Astrand P, Engquist B, Dahlgren S, et al. Astra tech and Branemark system implants: A 5-year prospective study of marginal bone reactions. Clin Oral Implants Res. 2004. 15:413–420.
Article25. Engquist B, Astrand P, Dahlgren S, et al. Marginal bone reaction to oral implants: A prospective comparative study of Astra tech and Branemark system implants. Clin Oral Implants Res. 2002. 13:30–37.26. Alomrani AN, Hermann JS, Jones AA, et al. The effect of a machined collar on coronal hard tissue around titanium implants: A radiographic study in the canine mandible. Int J Oral Maxillofac Implants. 2005. 20:677–686.27. Broggini N, McManus LM, Hermann JS, et al. Peri-implant inflammation defined by the implant-abutment interface. J Dent Res. 2006. 85:473–478.
Article28. Quirynen M, Bollen CM, Eyssen H, van Steenberghe D. Microbial penetration along the implant components of the Branemark system. an in vitro study. Clin Oral Implants Res. 1994. 5:239–244.
Article29. Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986. 1:11–25.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An 1 year prospective comparative study evaluating the effect of microthread on the maintenance of marginal bone level
- Radiographic evaluation of marginal bone resorption around two types of external hex implants: preliminary study
- Influence of microthread design on marginal cortical bone strain developement: A finite element analysis
- Study on radiographic evaluation of marginal bone loss around osseointegrated implant after functional loading
- Clinical, histologic, and histometric evaluation of implants with microthreaded crest module and SLA surface