Korean J Radiol.
2010 Apr;11(2):164-168. 10.3348/kjr.2010.11.2.164.
High-Resolution CT Findings of Re-Expansion Pulmonary Edema
- Affiliations
-
- 1Department of Radiology, St. Vincent's Hospital, The Catholic University of Korea, Seoul 137-701, Korea.
- 2Department of Radiology, Seoul St. Mary's Hospital, The Catholic University of Korea, Seoul 137-701, Korea. ami@catholic.ac.kr
- KMID: 1783192
- DOI: http://doi.org/10.3348/kjr.2010.11.2.164
Abstract
OBJECTIVE
To describe the high-resolution CT (HRCT) findings of re-expansion pulmonary edema (REPE) following a thoracentesis for a spontaneous pneumothorax.
MATERIALS AND METHODS
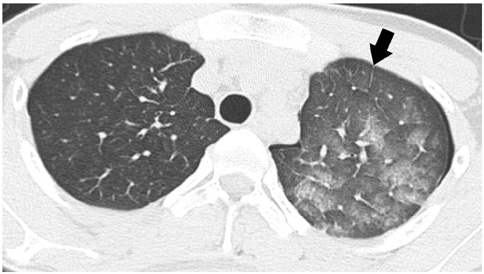
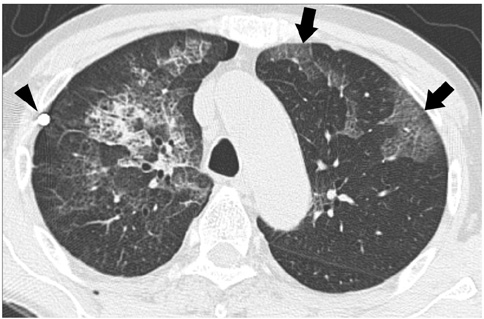
HRCT scans from 43 patients who developed REPE immediately after a thoracentesis for treatment of pneumothorax were retrospectively analyzed. The study group consisted of 41 men and two women with a mean age of 34 years. The average time interval between insertion of the drainage tube and HRCT was 8.5 hours (range, 1-24 hours). The patterns and distribution of the lung lesions were analyzed and were assigned one of the following classifications: consolidation, ground-glass opacity (GGO), intralobular interstitial thickening, interlobular septal thickening, thickening of bronchovascular bundles, and nodules. The presence of pleural effusion and contralateral lung involvement was also assessed.
RESULTS
Patchy areas of GGO were observed in all 43 patients examined. Consolidation was noted in 22 patients (51%). The geographic distribution of GGO and consolidation was noted in 25 patients (58%). Interlobular septal thickening and intralobular interstitial thickening was noted in 28 patients (65%), respectively. Bronchovascular bundle thickening was seen in 13 patients (30%), whereas ill-defined centrilobular GGO nodules were observed in five patients (12%). The lesions were predominantly peripheral in 38 patients (88%). Of these lesions, gravity-dependent distribution was noted in 23 cases (53%). Bilateral lung involvement was noted in four patients (9%), and a small amount of pleural effusion was seen in seven patients (16%).
CONCLUSION
The HRCT findings of REPE were peripheral patchy areas of GGO that were frequently combined with consolidation as well as interlobular septal and intralobular interstitial thickening.
Keyword
MeSH Terms
Figure
Reference
-
1. Mahfood S, Hix WR, Aaron BL, Blaes P, Watson DC. Reexpansion pulmonary edema. Ann Thorac Surg. 1988. 45:340–345.2. Matsuura Y, Nomimura T, Murakami H, Matsushima T, Kakehashi M, Kajihara H. Clinical analysis of reexpansion pulmonary edema. Chest. 1991. 100:1562–1566.3. Miller WC, Toon R, Palat H, Lacroix J. Experimental pulmonary edema following re-expansion of pneumothorax. Am Rev Respir Dis. 1973. 108:654–656.4. Sherman SC. Reexpansion pulmonary edema: a case report and review of the current literature. J Emerg Med. 2003. 24:23–27.5. Tarver RD, Broderick LS, Conces DJ Jr. Reexpansion pulmonary edema. J Thorac Imaging. 1996. 11:198–209.6. Gluecker T, Capasso P, Schnyder P, Gudinchet F, Schaller MD, Revelly JP, et al. Clinical and radiologic features of pulmonary edema. Radiographics. 1999. 19:1507–1531.7. Smolle-Juettner FM, Prause G, Ratzenhofer B, Pongratz M, Friehs G, List WF. The importance of early detection and therapy of reexpansion pulmonary edema. Thorac Cardiovasc Surg. 1991. 39:162–166.8. Humphreys RL, Berne AS. Rapid re-expansion of pneumothorax. A cause of unilateral pulmonary edema. Radiology. 1970. 96:509–512.9. Murat A, Arslan A, Balci AE. Re-expansion pulmonary edema. Acta Radiol. 2004. 45:431–433.10. Rozenman J, Yellin A, Simansky DA, Shiner RJ. Re-expansion pulmonary oedema following spontaneous pneumothorax. Respir Med. 1996. 90:235–238.11. Kim YK, Kim H, Lee CC, Choi HJ, Lee KH, Hwang SO, et al. New classification and clinical characteristics of reexpansion pulmonary edema after treatment of spontaneous pneumothorax. Am J Emerg Med. 2009. 27:961–967.12. Waqaruddin M, Bernstein A. Re-expansion pulmonary oedema. Thorax. 1975. 30:54–60.13. Woodring JH. Focal reexpansion pulmonary edema after drainage of large pleural effusions: clinical evidence suggesting hypoxic injury to the lung as the cause of edema. South Med J. 1997. 90:1176–1182.14. Maniwa K, Tanaka E, Inoue T, Sakuramoto M, Minakuchi M, Maeda Y, et al. Interstitial pulmonary edema revealed by high-resolution CT after relief of acute upper airway obstruction. Radiat Med. 2005. 23:139–141.15. Pavlin DJ, Nessly ML, Cheney FW. Increased pulmonary vascular permeability as a cause of re-expansion edema in rabbits. Am Rev Respir Dis. 1981. 124:422–427.16. Ketai LH, Godwin JD. A new view of pulmonary edema and acute respiratory distress syndrome. J Thorac Imaging. 1998. 13:147–171.17. Peatfield RC, Edwards PR, Johnson NM. Two unexpected deaths from pneumothorax. Lancet. 1979. 1:356–358.18. Heller BJ, Grathwohl MK. Contralateral reexpansion pulmonary edema. South Med J. 2000. 93:828–831.19. Ragozzino MW, Greene R. Bilateral reexpansion pulmonary edema following unilateral pleurocentesis. Chest. 1991. 99:506–508.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Experimentally Induced Fat Embolism in the Rabbit Lung: High-resolution CT and Pathologic Findings
- Acute Pulmonary Edema after Intravenous Administration of Nonionic Contrast Media: A Case Report
- Unilateral pulmonary edema following thoracotomy for the spontaneous pneumothorax
- High-Resolution CT Findings in Swyer-James Syndrome
- Unpredicted Sudden Onset of Postobstructive Pulmonary Edema Complicating Adenotonsillectomy in a Child