Korean J Radiol.
2006 Jun;7(2):131-138. 10.3348/kjr.2006.7.2.131.
Subintimal Angioplasty in the Treatment of Chronic Lower Limb Ischemia
- Affiliations
-
- 1Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ysdo@smc.samsung.co.kr
- 2Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1782186
- DOI: http://doi.org/10.3348/kjr.2006.7.2.131
Abstract
OBJECTIVE
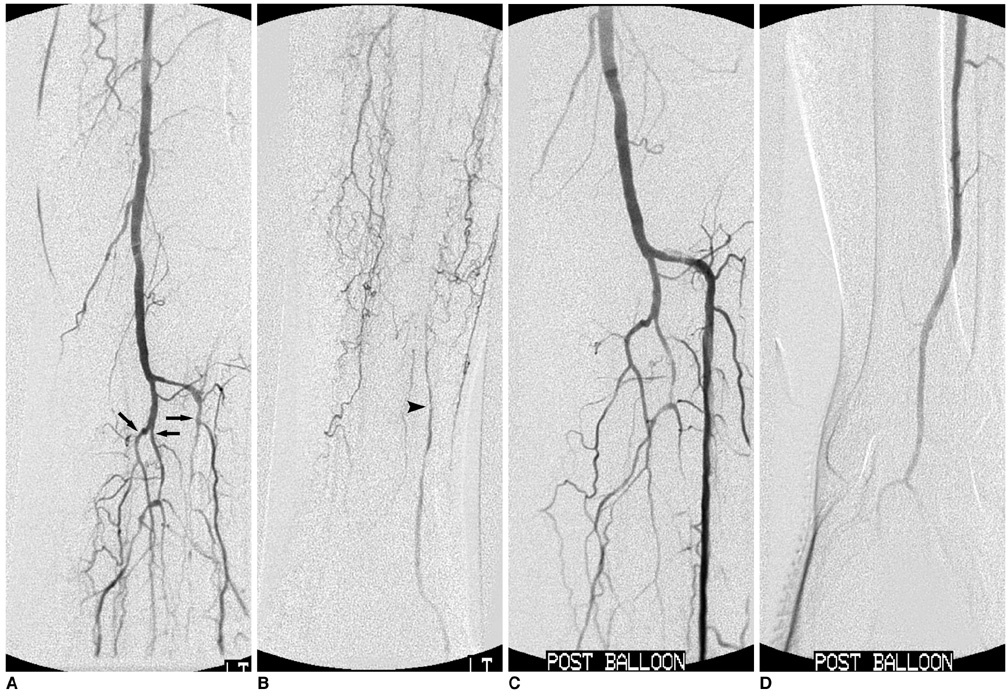
To present our experience with subintimal angioplasty (SA) for treatment of chronic lower limb ischemia (CLLI) and to assess its effectiveness and durability. MATERIALS AND METHODS: From April 2003 through June 2005, we treated 40 limbs in 36 patients with CLLI by SA. Balloons with or without secondary stent placement appropriate in size to the occluded arteries were used for SA of all lesions, except for iliac lesions where primary stent placement was done. The patients were followed for 1-23 months by clinical examination and color Doppler ultrasound and/or CT angiography. Technical results and outcomes were retrospectively evaluated. The presence of a steep learning curve for performance of SA was also evaluated. Primary and secondary patencies were determined using Kaplan-Meier analysis. RESULTS: Technical success was achieved in 32 (80%) of 40 limbs. There was no statistical difference between technical success rates of 75% (18/24) during the first year and 88% (14/16) thereafter. There were four complications (10%) in 40 procedures; two arterial perforations, one pseudoaneurysm at the puncture site, and one delayed hematoma at the SA site. Excluding initial technical failures, the primary patency rates at six and 12 months were 68% and 55%, respectively. Secondary patency rates at six and 12 months were 73% and 59%, respectively. CONCLUSION: Subintimal angioplasty can be accomplished with a high technical success rate. It should be attempted in patients with CLLI as an alternative to more extended surgery, or when surgical treatment is not recommended due to comorbidity or an unfavorable disease pattern.
MeSH Terms
Figure
Reference
-
1. Ashley S, Kester RC. Laser angioplasty. Br J Surg. 1993. 80:550–551.2. Bolia A, Miles KA, Brennan J, Bell PR. Percutaneous transluminal angioplasty of occlusions of the femoral and popliteal arteries by subintimal dissection. Cardiovasc Intervent Radiol. 1990. 13:357–363.3. Reekers JA. Short-term results of femoropopliteal subintimal angioplasty (Br J Surg 2000;87:1361-5). Br J Surg. 2001. 88:887–888.4. Bolia A. Percutaneous intentional extraluminal (subintimal) recanalization of crural arteries. Eur J Radiol. 1998. 28:199–204.5. Reekers JA, Bolia A. Percutaneous intentional extraluminal (subintimal) recanalization: how to do it yourself. Eur J Radiol. 1998. 28:192–198.6. Yilmaz S, Sindel T, Yegin A, Luleci E. Subintimal angioplasty of long superficial femoral artery occlusions. J Vasc Interv Radiol. 2003. 14:997–1010.7. Treiman GS, Whiting JH, Treiman RL, McNamara RM, Ashrafi A. Treatment of limb-threatening ischemia with percutaneous intentional extraluminal recanalization: a preliminary evaluation. J Vasc Surg. 2003. 38:29–35.8. Laxdal E, Jenssen GL, Pedersen G, Aune S. Subintimal angioplasty as a treatment of femoropopliteal artery occlusions. Eur J Vasc Endovasc Surg. 2003. 25:578–582.9. Lipsitz EC, Ohki T, Veith FJ, Suggs WD, Wain RA, Cynamon J, et al. Does subintimal angioplasty have a role in the treatment of severe lower extremity ischemia? J Vasc Surg. 2003. 37:386–391.10. Shaw MB, DeNunzio M, Hinwood D, Nash R, Callum KG, Braithwaite BD. The results of subintimal angioplasty in a district general hospital. Eur J Vasc Endovasc Surg. 2002. 24:524–527.11. Tisi PV, Mirnezami A, Baker S, Tawn J, Parvin SD, Darke SG. Role of subintimal angioplasty in the treatment of chronic lower limb ischaemia. Eur J Vasc Endovasc Surg. 2002. 24:417–422.12. Ingle H, Nasim A, Bolia A, Fishwick G, Naylor R, Bell PR, et al. Subintimal angioplasty of isolated infragenicular vessels in lower limb ischemia: long-term results. J Endovasc Ther. 2002. 9:411–416.13. Vraux H, Hammer F, Verhelst R, Goffette P, Vandeleene B. Subintimal angioplasty of tibial vessel occlusions in the treatment of critical limb ischaemia: mid-term results. Eur J Vasc Endovasc Surg. 2000. 20:441–446.14. McCarthy RJ, Neary W, Roobottom C, Tottle A, Ashley S. Short-term results of femoropopliteal subintimal angioplasty. Br J Surg. 2000. 87:1361–1365.15. Nydahl S, Hartshorne T, Bell PR, Bolia A, London NJ. Subintimal angioplasty of infrapopliteal occlusions in critically ischaemic limbs. Eur J Vasc Endovasc Surg. 1997. 14:212–216.16. London NJ, Srinivasan R, Naylor AR, Hartshorne T, Ratliff DA, Bell PR, et al. Subintimal angioplasty of femoropopliteal artery occlusions: the long-term results. Eur J Vasc Surg. 1994. 8:148–155.17. Bolia A, Bell PR. Femoropopliteal and crural artery recanalization using subintimal angioplasty. Semin Vasc Surg. 1995. 8:253–264.18. Desgranges P, Boufi M, Lapeyre M, Tarquini G, van Laere O, Losy F, et al. Subintimal angioplasty: feasible and durable. Eur J Vasc Endovasc Surg. 2004. 28:138–141.19. Lazaris AM, Tsiamis AC, Fishwick G, Bolia A, Bell PR. Clinical outcome of primary infrainguinal subintimal angioplasty in diabetic patients with critical lower limb ischemia. J Endovasc Ther. 2004. 11:447–453.20. Florenes T, Bay D, Sandbaek G, Saetre T, Jorgensen JJ, Slagsvold CE, et al. Subintimal angioplasty in the treatment of patients with intermittent claudication: long term results. Eur J Vasc Endovasc Surg. 2004. 28:645–650.21. Treiman GS. Subintimal angioplasty for infrainguinal occlusive disease. Surg Clin North Am. 2004. 84:1365–1380. viii.22. Heenan SD, Vinnicombe SJ, Buckenham TM, Belli AM. Percutaneous transluminal angioplasty by a retrograde subintimal transpopliteal approach. Clin Radiol. 1995. 50:507–508.23. Spinosa DJ, Leung DA, Harthun NL, Cage DL, Fritz Angle J, Hagspiel KD, et al. Simultaneous antegrade and retrograde access for subintimal recanalization of peripheral arterial occlusion. J Vasc Interv Radiol. 2003. 14:1449–1454.24. Balas P, Pangratis N, Ioannou N, Milas P, Klonaris C, Masouridou E. Open subintimal angioplasty of the superficial femoral and distal arteries. J Endovasc Ther. 2000. 7:68–71.25. Hausegger KA, Georgieva B, Portugaller H, Tauss J, Stark G. The outback catheter: a new device for true lumen re-entry after dissection during recanalization of arterial occlusions. Cardiovasc Intervent Radiol. 2004. 27:26–30.26. Willmann JK, Baumert B, Schertler T, Wildermuth S, Pfammatter T, Verdun FR, et al. Aortoiliac and lower extremity arteries assessed with 16-detector row CT angiography: prospective comparison with digital subtraction angiography. Radiology. 2005. 236:1083–1093.27. Nadal LL, Cynamon J, Lipsitz EC, Bolia A. Subintimal angioplasty for chronic arterial occlusions. Tech Vasc Interv Radiol. 2004. 7:16–22.28. Wright G, Fishwick G, Naylor AR. Arterial perforation (by balloon) during subintimal angioplasty. Eur J Vasc Endovasc Surg. 2004. 28:108–110.29. Brookes JA, Aly S, Bishop CC. Re: arterial perforation (by balloon) during subintimal angioplasty by Dr Wright and colleagues from Leicester Royal Infirmary, Leicester, United Kingdom published in Eur J Vasc Endovasc Surg 28, 108-110 (2004). Eur J Vasc Endovasc Surg. 2004. 28:677–678.30. Ouriel K. A critical review of subintimal angioplasty. Vascular News. 2003. . London: BIBA Publishing;15–16.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of subintimal balloon angioplasty in Buerger's disease
- The Early Outcome of the Endovascular Subintimal Angioplasty for Chronic Critical Limb Ischemia in Infrainguinal Vascular Disease
- Successful Recanalization of a Long Superficial Femoral Artery Occlusion by Retrograde Subintimal Angioplasty After a Failed Antegrade Subintimal Approach
- RE: Percutaneous Angioplasty in Diabetic Patients with Critical Limb Ischemia
- General Treatment Strategy for Intervention in Lower Extremity Arterial Disease