J Korean Med Sci.
2009 Oct;24(5):989-991. 10.3346/jkms.2009.24.5.989.
A Primary Extragonadal Teratoma of the Proximal Humerus
- Affiliations
-
- 1Department of Pathology, Korea Cancer Center Hospital, Seoul, Korea.
- 2Department of Orthopedic Surgery, Korea University Anam Hospital, Seoul, Korea. pjh1964@hanmail.net
- 3Department of Radiology, Korea University Anam Hospital, Seoul, Korea.
- KMID: 1782031
- DOI: http://doi.org/10.3346/jkms.2009.24.5.989
Abstract
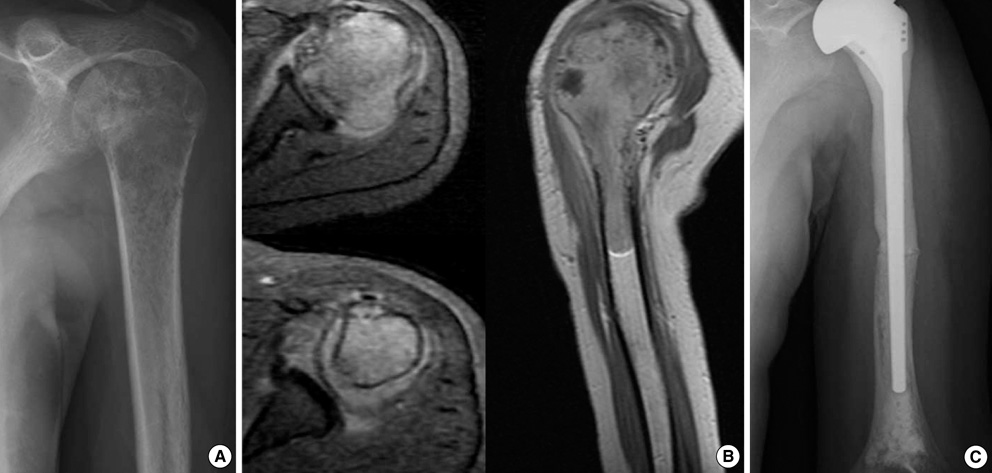
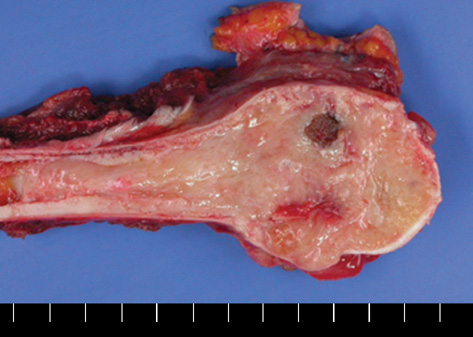
- A extragonadal malignant teratoma of the extremity is a rare pheonemenon. We describe a extremely rare case of malignant teratoma of the left proximal humerus in a 14-yr-old female. Radiologic evaluations, including magnetic resonance imaging, suggested a malignant bone tumor, but a pathological examination revealed an immature bony teratoma. Bone scintigraphy and positron emission tomography computed tomography scan showed increased uptake of proximal humerus but no other abnormal lesion.
Keyword
MeSH Terms
Figure
Reference
-
1. Robboy SJ, Scully RE. Ovarian teratoma with glial implants on the peritoneum. An analysis of 12 cases. Hum Pathol. 1970. 1:643–653.2. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993. 286:241–246.
Article3. Gatcombe HG, Assikis V, Kooby D, Johnstone PA. Primary retroperitoneal teratomas: a review of the literature. J Surg Oncol. 2004. 86:107–113.
Article4. Batsakis JG, el-Naggar AK, Luna MA. Teratomas of the head and neck with emphasis on malignancy. Ann Otol Rhinol Laryngol. 1995. 104:496–500.
Article5. Taori K, Rathod J, Deshmukh A, Sheorain VS, Jawale R, Sanyal R, Bhagat M, Jumle S. Primary extragonadal retroperitoneal teratoma in an adult. Br J Radiol. 2006. 79:e120–e122.
Article6. Chinoy RF, Soman CS, Swaroop D, Badwar RA. Extragonadal malignant teratoma of the foot. Indian J Cancer. 1992. 29:96–99.7. Vazquez JL, Jaramillo D, Gebhardt MC, Perez-Atayde AR. Intraosseus teratoma of the iliac bone. Pediatr Radiol. 2000. 30:258–261.
Article8. Baumann FR, Nerlich A. Metastasizing cervical teratoma of the fetus. Pediatr Pathol. 1993. 13:21–27.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Homogenous Osteoarticular Transplantation of the Proximal Humerus: Report of A Case
- Primary Retroperitoneal Teratoma: A Case Report
- Early Intrathoracic Migration of K-wire Used for Fixation of Proximal Humerus Fracture
- One Case of Primary Extragonadal Germ Cell Tumor of Retroperitoneal Origin
- Two Cases of Extragonadal Embryonal Carcinoma Originating in Unusual Sites