Yonsei Med J.
2014 Jan;55(1):149-156. 10.3349/ymj.2014.55.1.149.
Three-Year Experience of Pouch Dilatation and Slippage Management after Laparoscopic Adjustable Gastric Banding
- Affiliations
-
- 1Department of Surgery, Gil Medical Center, Gachon University of Medicine, Incheon, Korea. seongmin_kim@gilhospital.com
- KMID: 1779899
- DOI: http://doi.org/10.3349/ymj.2014.55.1.149
Abstract
- PURPOSE
Pouch dilatation and band slippage are the most common long-term complications after laparoscopic adjustable gastric banding (LAGB). The aim of the study is to present our experience of diagnosis and management of these complications.
MATERIALS AND METHODS
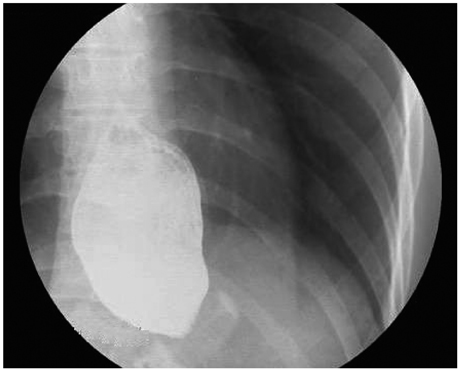
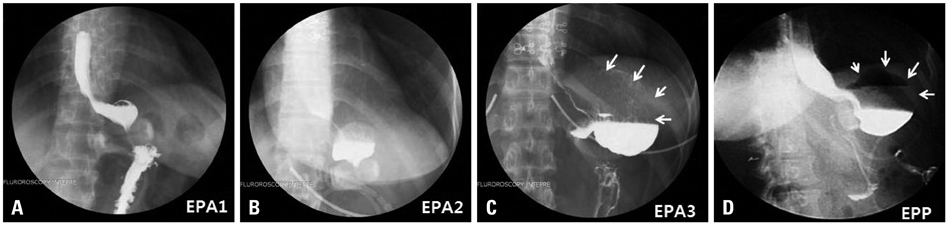
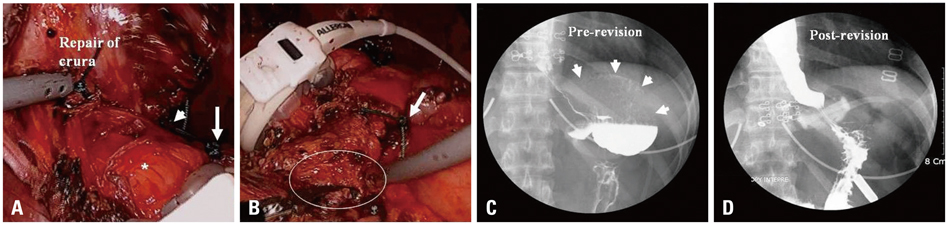
The pars flaccida technique with anterior fixation of the fundus was routinely used. All band adjustments were performed under fluoroscopy. We analyzed the incidence, clinico-radiologic features, management, and revisional surgeries for treatment of these complications. We further presented the outcome of gastric plication techniques as a measure for prevention of these complications.
RESULTS
From March 2009 to March 2012, we performed LAGB on 126 morbidly obese patients. Among them, 14 patients (11.1%) were diagnosed as having these complications. Four patients (3.2%) had concentric pouch dilatations, which were corrected by band adjustment. Ten (7.9%) had eccentric pouch with band slippage. Among the ten patients, there were three cases of posterior slippage, which were corrected by reoperation, and seven cases of eccentric pouch dilatation with anterior slippage. Three were early anterior slippage, which was managed conservatively. Two were acute anterior slippage, one of whom underwent a revision. There were two cases of chronic anterior slippage, one of whom underwent a revision. The 27 patients who underwent gastric plication did not present with eccentric pouch with band slippage during the follow-up period.
CONCLUSION
The incidence of pouch dilatation with/without band slippage was 11.1%. Management should be individualized according to clinico-radiologic patterns. Gastric plication below the band might prevent these complications.
MeSH Terms
Figure
Cited by 2 articles
-
Short-Term Analysis of Food Tolerance and Quality of Life after Laparoscopic Greater Curvature Plication
Su Bin Kim, Seong Min Kim
Yonsei Med J. 2016;57(2):430-440. doi: 10.3349/ymj.2016.57.2.430.Explantation of Adjustable Gastric Bands: An Observation Study of 10 Years of Experience at a Tertiary Center
Eun Jung Cho, Seong Min Kim
Yonsei Med J. 2019;60(8):782-790. doi: 10.3349/ymj.2019.60.8.782.
Reference
-
1. Tolonen P, Victorzon M, Mäkelä J. 11-year experience with laparoscopic adjustable gastric banding for morbid obesity--what happened to the first 123 patients? Obes Surg. 2008; 18:251–255.
Article2. Himpens J, Cadière GB, Bazi M, Vouche M, Cadière B, Dapri G. Long-term outcomes of laparoscopic adjustable gastric banding. Arch Surg. 2011; 146:802–807.
Article3. Suter M, Calmes JM, Paroz A, Giusti V. A 10-year experience with laparoscopic gastric banding for morbid obesity: high long-term complication and failure rates. Obes Surg. 2006; 16:829–835.
Article4. Stroh C, Hohmann U, Schramm H, Meyer F, Manger T. Fourteen-year long-term results after gastric banding. J Obes. 2011; 2011:128451.
Article5. Kriwanek S, Schermann M, Ali Abdullah S, Roka R. Band slippage--a potentially life-threatening complication after laparoscopic adjustable gastric banding. Obes Surg. 2005; 15:133–136.
Article6. Hofer M, Stöllberger C, Finsterer J, Kriwanek S. Recurrent aspiration pneumonia after laparoscopic adjustable gastric banding. Obes Surg. 2007; 17:565–567.
Article7. Yoon CI, Pak KH, Kim SM. Early experience with diagnosis and management of eroded gastric bands. J Korean Surg Soc. 2012; 82:18–27.
Article8. Seo WJ, Pak KH, Kim SM. Novel method for port implantation in lap-band surgery--transumbilical subfascial port implantation. J Laparoendosc Adv Surg Tech A. 2012; 22:254–258.
Article9. Fielding GA, Allen JW. A step-by-step guide to placement of the LAP-BAND adjustable gastric banding system. Am J Surg. 2002; 184:26S–30S.
Article10. Ponce J, Paynter S, Fromm R. Laparoscopic adjustable gastric banding: 1,014 consecutive cases. J Am Coll Surg. 2005; 201:529–535.
Article11. Vertruyen M. Repositioning the Lap-Band for proximal pouch dilatation. Obes Surg. 2003; 13:285–288.
Article12. Manganiello M, Sarker S, Tempel M, Shayani V. Management of slipped adjustable gastric bands. Surg Obes Relat Dis. 2008; 4:534–538.
Article13. Moser F, Gorodner MV, Galvani CA, Baptista M, Chretien C, Horgan S. Pouch enlargement and band slippage: two different entities. Surg Endosc. 2006; 20:1021–1029.
Article14. Sherwinter DA, Powers CJ, Geiss AC, Howard M, Warman J. Posterior prolapse: an important entity even in the modern age of the pars flaccida approach to lap-band placement. Obes Surg. 2006; 16:1312–1317.
Article15. Egan RJ, Monkhouse SJ, Meredith HE, Bates SE, Morgan JD, Norton SA. The reporting of gastric band slip and related complications; a review of the literature. Obes Surg. 2011; 21:1280–1288.
Article16. Brown WA, Burton PR, Anderson M, Korin A, Dixon JB, Hebbard G, et al. Symmetrical pouch dilatation after laparoscopic adjustable gastric banding: incidence and management. Obes Surg. 2008; 18:1104–1108.
Article17. Avsar FM, Sakcak I, Yildiz BD, Cosgun E, Hamamci EO. Is gastro-gastric fixation suture necessary in laparoscopic adjustable gastric banding? A prospective randomized study. J Laparoendosc Adv Surg Tech A. 2011; 21:953–956.
Article18. Fried M, Dolezalova K, Sramkova P. Adjustable gastric banding outcomes with and without gastrogastric imbrication sutures: a randomized controlled trial. Surg Obes Relat Dis. 2011; 7:23–31.
Article19. Lazzati A, Polliand C, Porta M, Torcivia A, Paolino LA, Champault G, et al. Is fixation during gastric banding necessary? A randomised clinical study. Obes Surg. 2011; 21:1859–1863.
Article20. Keidar A, Szold A, Carmon E, Blanc A, Abu-Abeid S. Band slippage after laparoscopic adjustable gastric banding: etiology and treatment. Surg Endosc. 2005; 19:262–267.
Article21. O'Brien PE, Dixon JB. Laparoscopic adjustable gastric banding in the treatment of morbid obesity. Arch Surg. 2003; 138:376–382.22. Wiesner W, Schöb O, Hauser RS, Hauser M. Adjustable laparoscopic gastric banding in patients with morbid obesity: radiographic management, results, and postoperative complications. Radiology. 2000; 216:389–394.
Article23. Carucci LR, Turner MA, Szucs RA. Adjustable laparoscopic gastric banding for morbid obesity: imaging assessment and complications. Radiol Clin North Am. 2007; 45:261–274.
Article24. Chevallier JM, Zinzindohoué F, Elian N, Cherrak A, Blanche JP, Berta JL, et al. Adjustable gastric banding in a public university hospital: prospective analysis of 400 patients. Obes Surg. 2002; 12:93–99.
Article25. Suter M, Bettschart V, Giusti V, Heraief E, Jayet A. A 3-year experience with laparoscopic gastric banding for obesity. Surg Endosc. 2000; 14:532–536.
Article26. Suter M. Laparoscopic band repositioning for pouch dilatation/slippage after gastric banding: disappointing results. Obes Surg. 2001; 11:507–512.
Article27. Foletto M, Bernante P, Busetto L, Pomerri F, Vecchiato G, Prevedello L, et al. Laparoscopic gastric rebanding for slippage with pouch dilation: results on 29 consecutive patients. Obes Surg. 2008; 18:1099–1103.
Article28. Srikanth MS, Oh KH, Keskey T, Rumbaut R, Fox SR, Fox ER, et al. Critical extreme anterior slippage (paragastric Richter's hernia) of the stomach after laparoscopic adjustable gastric banding: early recognition and prevention of gastric strangulation. Obes Surg. 2005; 15:207–215.
Article29. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363:157–163.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Band Slippage after Laparoscopic Adjustable Gastric Banding (LAGB)
- Conversion Sleeve Gastrectomy for Pouch Dilatation and Band Scar Stenosis: 1 Case
- Pulmonary aspiration during anesthetic induction in a patient with laparoscopic adjustable gastric band: A case report
- Case Report: Superior Mesenteric Artery Syndrome following Laparoscopic Adjustable Gastric Banding
- Acute Gastric Band Slippage During the 3rd Trimester Gestation