Yonsei Med J.
2010 Nov;51(6):932-937. 10.3349/ymj.2010.51.6.932.
Clinical Features and Treatments of Odontogenic Sinusitis
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. fess0101@hanmail.net
- KMID: 1779642
- DOI: http://doi.org/10.3349/ymj.2010.51.6.932
Abstract
- PURPOSE
The aim of this study was to investigate how clinical features such as sex, age, etiologic factors, and presenting symptoms of odontogenic sinusitis are differentiated from other types of sinusitis. Also, this study was designed to find methods for reducing the incidence of odontogenic sinusitis.
MATERIALS AND METHODS
A retrospective chart analysis was completed on twenty-seven patients with odontogenic sinusitis. They were all treated at Kangbuk Samsung Hospital between February 2006 and August 2008. The study protocol and informed consent forms were approved by the institutional review boards for human beings at Kangbuk Samsung Hospital.
RESULTS
Ten patients (37.0%) had dental implant related complications and 8 (29.6%) had dental extraction related complications. Unilateral purulent nasal discharge was the most common symptom (66.7%). The therapeutic modality included transnasal endoscopic sinus surgery in 19 (70.4%) patients, and a Caldwell-Luc operation in two (7.4%) patients.
CONCLUSION
In our study, there was no significant difference in the incidence between genders. The average age of the patients was 42.9 years. The incidence was highest in the fourth decade. There were no significant differences between the symptoms of odontogenic sinusitis and that of other types of sinusitis. However, almost all of the patients with odontogenic sinusitis had unilateral symptoms. Iatrogenic causes, which include dental implants and dental extractions, were the most common etiologic factors related to the development of odontogenic sinusitis. Therefore, a preoperative consultation between a rhinologist and a dentist prior to the dental procedure should be able to reduce the incidence of odontogenic sinusitis.
MeSH Terms
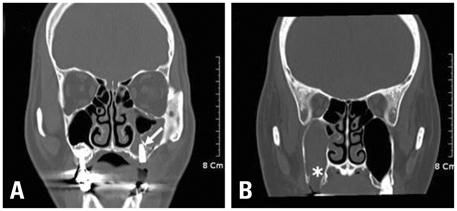
Figure
Cited by 2 articles
-
Analysis of Treatment Outcome Associated with Pre-Operative Diagnostic Accuracy Changes and Dental Treatment Timing in Odontogenic Sinusitis Involving Unilateral Maxillary Sinus
Ki-Yong Choi, Ji-Hun Mo, Young-Jun Chung
Korean J Otorhinolaryngol-Head Neck Surg. 2019;62(11):624-630. doi: 10.3342/kjorl-hns.2018.00703.Clinical Characteristics of Patients Diagnosed With Odontogenic Rhinosinusitis After Dental Implants
Sangjun Kim, Eun Soo Lee, Woo Yong Bae, Chul-Hoon Kim, Ji-Eon Yun
J Rhinol. 2022;29(1):13-18. doi: 10.18787/jr.2021.00380.
Reference
-
1. Lopatin AS, Sysolyatin SP, Sysolyatin PG, Melnikov MN. Chronic maxillary sinusitis of dental origin: is external surgical approach mandatory? Laryngoscope. 2002. 112:1056–1059.
Article2. Mehra P, Murad H. Maxillary sinus disease of odontogenic origin. Otolaryngol Clin North Am. 2004. 37:347–364.
Article3. Kretzschmar DP, Kretzschmar JL. Rhinosinusitis: review from a dental perspective. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003. 96:128–135.
Article4. Timmenga NM, Raghoebar GM, Boering G, van Weissenbruch R. Maxillary sinus function after sinus lifts for the insertion of dental implants. J Oral Maxillofac Surg. 1997. 55:936–939.
Article5. Kaneko I, Harada K, Ishii T, Furukawa K, Yao K, Takahashi H, et al. [Clinical feature of odontogenic maxillary sinusitis--symptomatology and the grade in development of the maxillary sinus in cases of dental maxillary sinusitis]. Nippon Jibiinkoka Gakkai Kaiho. 1990. 93:1034–1040.
Article6. Ugincius P, Kubilius R, Gervickas A, Vaitkus S. Chronic odontogenic maxillary sinusitis. Stomatologija. 2006. 8:44–48.7. Lin PT, Bukachevsky R, Blake M. Management of odontongenic sinusitis with persistent oro-antral fistula. Ear Nose Throat J. 1991. 70:488–490.8. Yoshiura K, Ban S, Hijiya T, Yuasa K, Miwa K, Ariji E, et al. Analysis of maxillary sinusitis using computed tomography. Dentomaxillofac Radiol. 1993. 22:86–92.
Article9. Konen E, Faibel M, Kleinbaum Y, Wolf M, Lusky A, Hoffman C, et al. The value of the occipitomental (Water's) view in diagnosis of sinusitis: A comparative study with computed tomography. Clin Radiol. 2000. 55:856–860.
Article10. Regev E, Smith RA, Perrott DH, Pogrel MA. Maxillary sinus complications related to endosseous implants. Int J Oral Maxillofac Implants. 1995. 10:451–461.11. Ueda M, Kaneda T. Maxillary sinusitis caused by dental implants: report of two cases. J Oral Maxillofac Surg. 1992. 50:285–287.
Article12. Quiney RE, Brimble M, Hodge M. Maxillary sinusitis from dental osseointegrated implants. J Laryngol Otol. 1990. 104:333–334.
Article13. Güneri P, Kaya A, Caliskan MK. Antroliths: survey of the literature and a report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005. 99:517–521.14. Sato K. [Pathology of recent odontogenic maxillary sinusitis and the usefulness of endoscopic sinus surgery]. Nippon Jibiinkoka Gakkai Kaiho. 2001. 104:715–720.15. Iida S, Tanaka N, Kogo M, Matsuya T. Migration of a dental implant into the maxillary sinus. A case report. Int J Oral Maxillofac Surg. 2000. 29:358–359.16. Block MS, Kent JN. Maxillary sinus grafting for totally and partially edentulous patients. J Am Dent Assoc. 1993. 124:139–143.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of Treatment Outcome Associated with Pre-Operative Diagnostic Accuracy Changes and Dental Treatment Timing in Odontogenic Sinusitis Involving Unilateral Maxillary Sinus
- Clinical Manifestation of Odontogenic Sinusitis : As to Pathophysiology and Management
- Recent Trends of Prevalence in Unilateral Sinusitis and Useful Factors in Differential Diagnosis
- Definition and management of odontogenic maxillary sinusitis
- Functional endoscopic sinus surgery for odontogenic maxillary sinusitis; A case report