J Korean Med Sci.
2007 Jun;22(3):588-594. 10.3346/jkms.2007.22.3.588.
Successful Combined Treatment with Total Parenteral Nutrition Fluid Extravasation Injuries in Preterm Infants
- Affiliations
-
- 1Department of Pediatrics, Ewha Womans University College of Medicine, 911-1 Mok-dong, Yangcheon-gu, Seoul, Korea. pea8639@ewha.ac.kr
- 2Department of Plastic Surgery, Ewha Womans University College of Medicine, Seoul, Korea.
- KMID: 1778379
- DOI: http://doi.org/10.3346/jkms.2007.22.3.588
Abstract
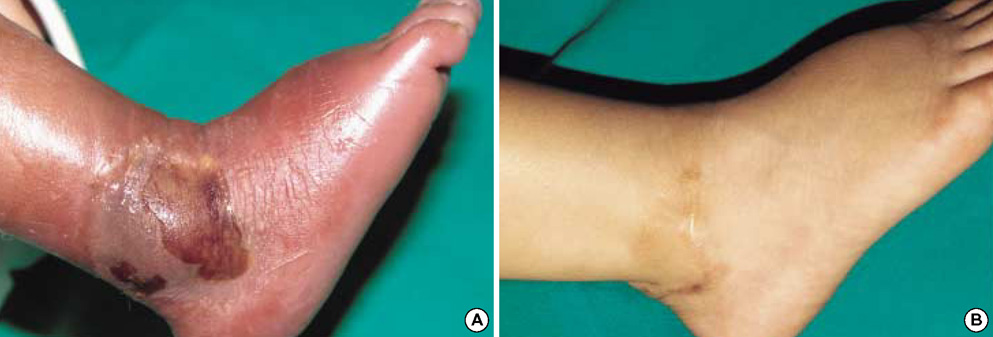
- Extravasation injuries in the neonatal intensive care unit are not rare during parenteral hyperalimentation. There have been many different methods of management. We report five premature infants with wounds of hyperalimentation fluid extravasation managed by the antibacterial ointment (Terramycin ophthalmic ointment(TM)) and sesame oil and a antiinflammatory herbal mixture (MEBO(TM)). The mean gestational age of patients was 31(+2) weeks (range, 28(+4) to 35(+6) weeks), and the mean weight at extravasation was 1,930 g (range, 1,140 to 2,680 g). Extravasation occurred within the mean of 32 days (range, 17 to 50 days). The method of dressing was application of a thick layer of this mixture covered by vaseline and wet gauze renewed at an interval of 8-12 hr after irrigating the wounds thoroughly with normal saline. The mean duration of dressing was 30 days (range, 20-50 days). The wounds had healed completely leaving a small size of contracture without functional abnormality. We conclude that this therapy may be considered for an alternative treatment and warrants clinical trials for the confirmation of the local management of extravasation injury.
Keyword
MeSH Terms
-
Administration, Topical
Anti-Bacterial Agents/*administration & dosage
Extravasation of Diagnostic and Therapeutic Materials/*therapy
Humans
Infant
Infant, Newborn
Infant, Premature
Infant, Premature, Diseases/*therapy
Ointments
Oxytetracycline/*administration & dosage
Parenteral Nutrition
Phytotherapy/methods
Treatment Outcome
Veins/*injuries
Wound Healing
Figure
Reference
-
1. Yosowitz P, Ekland DA, Shaw RC, Parsons RW. Peripheral intravenous infiltration necrosis. Ann Surg. 1975. 182:553–556.
Article2. Brown AS, Hoelzer DJ, Piercy SA. Skin necrosis from extravasation of intravenous fluids in children. Plast Reconstr Surg. 1979. 64:145–150.
Article3. Kumar RJ, Pegg SP, Kimble RM. Management of extravasation injuries. ANZ J Surg. 2001. 71:285–289.
Article4. Zhang HQ, Yip TP, Hui I, Lai V, Wong A. Efficacy of moist exposed burn ointment on burns. J Burn Care Rehabil. 2005. 26:247–251.5. Xu RX. Clinical uses of moist exposure therapy of burn. Zhong Xi Yi Jie He Za Zhi. 1988. 8:204–206.6. Atiyeh BS, Ioannovich J, Magliacani G, Masellis M, Costagliola M, Dham R, Al-Musa KA. A new approach to local burn wound care: moist exposed therapy. A multiphase, multicenter study. J Burns Wound Care. 2003. 2:18–27.7. Moon EJ, Lee YM, Lee OH, Lee MJ, Lee SK, Chung MH, Park YI, Sung CK, Choi JS, Kim KW. A novel angiogenic factor derived from Aloe vera gel: beta-sitosterol, a plant sterol. Angiogenesis. 1999. 3:117–123.8. Salatino A, Teixeira EW, Negri G, Message D. Origin and chemical variation of brazilian propolis. Evid Based Complement Alternat Med. 2005. 2:33–38.
Article9. Atiyeh BS, Ioannovich J, Magliacani G, Masellis M, Costagliola M, Dham R. Efficacy of moist exposed burn ointment in the management of cutaneous wounds and ulcers: a multicenter pilot study. Ann Plast Surg. 2002. 48:226–227.
Article10. Wilkins CE, Emmerson AJ. Extravasation injuries on regional neonatal units. Arch Dis Child Fetal Neonatal Ed. 2004. 89:274–275.
Article11. Cartildge PH, Fox PE, Rutter N. The scars of newborn intensive care. Early Hum Dev. 1990. 21:1–10.12. Atiyeh BS, EI-Musa KA, Dham R. Scar quality and physiologic barrier function restoration after moist and moist-exposed dressings of partial-thickness wounds. Dermatol Surg. 2003. 29:14–20.
Article13. Lionelli GT, Lawrence WT. Wound dressings. Surg Clin North Am. 2003. 83:617–638.
Article14. Ait-Aissa M. Advances in the use of SESAME OIL MIXTURE (a new approach in the method of application). Annal of Burns and Fire disasters. 2002. 15:1–4.15. Atiyeh BS, Dham R, Costagliola M, Al-Amm CA, Belhaouari L. Moist exposed therapy: an effective and valid alternative to occlusive dressings for postlaser resurfacing wound care. Dermatol Surg. 2004. 30:18–25.
Article16. Upton J, Mulliken JB, Murray JE. Major intravenous extravasation injuries. Am J Surg. 1979. 137:497–506.
Article17. Lynch DJ, Key JC, White RR. Management and prevention of infiltration and extravasation injury. Surg Clin North Am. 1979. 59:939–949.
Article18. Gault DT. Extravastion injuries. Br J Plast Surg. 1993. 46:91–96.19. Heckler FR. Current thoughts on extravasation injuries. Clin Plast Surg. 1989. 16:557–563.
Article20. Harris PA, Bradley S, Moss AL. Limiting the damage of iatrogenic extravasation injury in neonates. Plast Reconstr Surg. 2001. 107:893–894.
Article21. Hermansen MC, Hermansen MG. Intravascular catheter complications in the neonatal intensive care unit. Clin Perinatol. 2005. 32:141–156.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Parenteral Nutrition Support in Preterm Infants
- Enteral Feeding for Preterm Infants-Benefits and Risks
- The Effect of Parenteral Nutrition and Respiratory Distress Syndrome in the Early Neonatal Period on Bone Mineralization at the Time of Reaching 2 kg Body Weight in Premature Infants
- Umbilical Venous Catheter Complication Presenting as Chylous Ascites in a Newborn: Intraperitoneal Extravasation of Total Parenteral Nutrition Infusate
- Compartment syndrome due to extravasation of peripheral parenteral nutrition: extravasation injury of parenteral nutrition