J Korean Med Sci.
2007 Jun;22(3):476-483. 10.3346/jkms.2007.22.3.476.
Two Methods of Setting Positive End-expiratory Pressure in Acute Lung Injury: An Experimental Computed Tomography Volumetric Study
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, 50 Irwon-dong, Gangnam-gu, Seoul, Korea. gysuh@smc.samsung.co.kr
- 2Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Radiology, Seoul National University Bundang Hospital, Korea.
- KMID: 1778357
- DOI: http://doi.org/10.3346/jkms.2007.22.3.476
Abstract
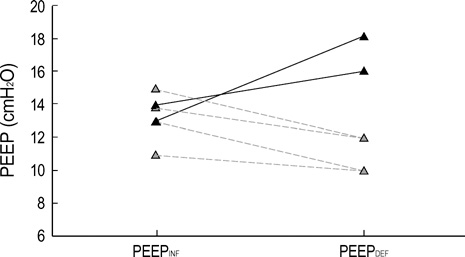
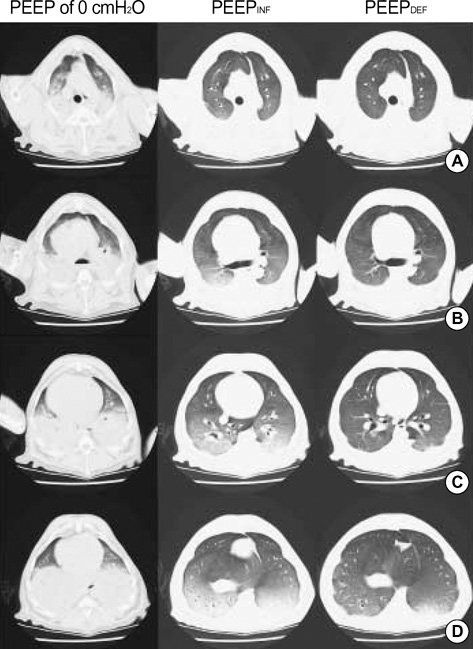
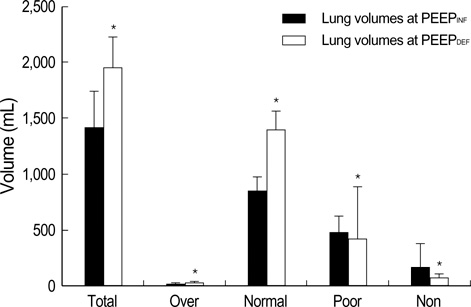
- This study was conducted to observe effects of two methods of setting positive endexpiratory pressure (PEEP) based on the pressure-volume (PV) curve. After lung injury was induced by oleic acid in six mongrel adult dogs, the inflation PV curve was traced and the lower inflection point (LIP) was measured. The 'PEEP(INF)' was defined as LIP+2 cmH2O. After recruitment maneuver to move the lung physiology to the deflation limb of PV curve, decremental PEEP was applied. The lowest level of PEEP that did not result in a significant drop in PaO2 was defined as the 'PEEP(DEF)'. Arterial blood gases, lung mechanics, hemodynamics, and lung volumes (measured on computed tomography during end-expiratory pause) were measured at PEEP of 0 cmH2O, PEEP(INF) and PEEP(DEF) sequentially. The median PEEP(INF) was 13.4 cm H2O (interquartile range, 12.5-14.3) and median PEEP(DEF) was 12.0 cm H2O (10.0-16.5) (p=0.813). PEEP(DEF) was associated with significantly higher PaO2 and lung volumes, and significantly lower shunt fraction and cardiac index when compared to PEEP(INF) (p<0.05). Setting the PEEP based on the deflation limb of the PV curve was useful in improving oxygenation and lung volumes in a canine lung injury model.
Keyword
MeSH Terms
Figure
Reference
-
1. Dreyfuss D, Saumon G. Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med. 1998. 157:294–323.2. International consensus conferences in intensive care medicine: Ventilator-associated Lung Injury in ARDS. This official conference report was cosponsored by the American Thoracic Society, The European Society of Intensive Care Medicine, and The Societe de Reanimation de Langue Francaise, and was approved by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med. 1999. 160:2118–2124.3. Marini JJ, Gattinoni L. Ventilatory management of acute respiratory distress syndrome: a consensus of two. Crit Care Med. 2004. 32:250–255.
Article4. Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, Takagaki TY, Carvalho CR. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998. 338:347–354.
Article5. Ranieri VM, Suter PM, Tortorella C, De Tullio R, Dayer JM, Brienza A, Bruno F, Slutsky AS. Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: a randomized controlled trial. JAMA. 1999. 282:54–61.
Article6. The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000. 342:1301–1308.7. Gattinoni L, D'Andrea L, Pelosi P, Vitale G, Pesenti A, Fumagalli R. Regional effects and mechanism of positive end-expiratory pressure in early adult respiratory distress syndrome. JAMA. 1993. 269:2122–2127.
Article8. Muscedere JG, Mullen JB, Gan K, Slutsky AS. Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med. 1994. 149:1327–1334.
Article9. Eisner MD, Thompson BT, Schoenfeld D, Anzueto A, Matthay MA. Airway pressures and early barotrauma in patients with acute lung injury and acute respiratory distress syndrome. Am J Respir Crit Care Med. 2002. 165:978–982.
Article10. Holzapfel L, Robert D, Perrin F, Blanc PL, Palmier B, Guerin C. Static pressure-volume curves and effect of positive end-expiratory pressure on gas exchange in adult respiratory distress syndrome. Crit Care Med. 1983. 11:591–597.
Article11. Amato MB, Barbas CS, Medeiros DM, Schettino Gde P, Lorenzi Filho G, Kairalla RA, Deheinzelin D, Morais C, Fernandes Ede O, Takagaki TY. Beneficial effects of the "open lung approach" with low distending pressures in acute respiratory distress syndrome. A prospective randomized study on mechanical ventilation. Am J Respir Crit Care Med. 1995. 152:1835–1846.
Article12. Matamis D, Lemaire F, Harf A, Brun-Buisson C, Ansquer JC, Atlan G. Total respiratory pressure-volume curves in the adult respiratory distress syndrome. Chest. 1984. 86:58–66.
Article13. Suter PM, Fairley B, Isenberg MD. Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N Engl J Med. 1975. 292:284–289.
Article14. Suh GY, Kwon OJ, Yoon JW, Park SJ, Ham HS, Kang SJ, Koh WJ, Chung MP, Kim HJ. A practical protocol for titrating "optimal" PEEP in acute lung injury: recruitment maneuver and PEEP decrement. J Korean Med Sci. 2003. 18:349–354.
Article15. Takeuchi M, Goddon S, Dolhnikoff M, Shimaoka M, Hess D, Amato MB, Kacmarek RM. Set positive end-expiratory pressure during protective ventilation affects lung injury. Anesthesiology. 2002. 97:682–692.
Article16. Albaiceta GM, Taboada F, Parra D, Luyando LH, Calvo J, Menendez R, Otero J. Tomographic study of the inflection points of the pressure-volume curve in acute lung injury. Am J Respir Crit Care Med. 2004. 170:1066–1072.
Article17. Suh GY, Chung MP, Park SJ, Park JW, Kim HC, Kim H, Han J, Rhee CH, Kwon OJ. Partial liquid ventilation with perfluorocarbon improves gas exchange and decreases inflammatory response in oleic acid-induced lung injury in beagles. J Korean Med Sci. 1999. 14:613–622.
Article18. Fernandez R, Blanch L, Artigas A. Inflation static pressure-volume curves of the total respiratory system determined without any instrumentation other than the mechanical ventilator. Intensive Care Med. 1993. 19:33–38.
Article19. Suh GY, Koh Y, Chung MP, An CH, Kim H, Jang WY, Han J, Kwon OJ. Repeated derecruitments accentuate lung injury during mechanical ventilation. Crit Care Med. 2002. 30:1848–1853.
Article20. Puybasset L, Cluzel P, Gusman P, Grenier P, Preteux F, Rouby JJ. Regional distribution of gas and tissue in acute respiratory distress syndrome. I. Consequences for lung morphology. CT Scan ARDS Study Group. Intensive Care Med. 2000. 26:857–869.21. Munro BH. Munro BH, editor. Selected nonparametric techniques. Statistical methods for health care research. 2000. 4th ed. Philadelphia: Lippincott Williams & Wilkins.22. Brochard L. Tobin MJ, editor. Respiratory pressure-volume curves. Principles and practice of intensive care monitoring. 1997. New York, NY: McGraw-Hill;597–616.23. Crotti S, Mascheroni D, Caironi P, Pelosi P, Ronzoni G, Mondino M, Marini JJ, Gattinoni L. Recruitment and derecruitment during acute respiratory failure: a clinical study. Am J Respir Crit Care Med. 2001. 164:131–140.24. Maggiore SM, Jonson B, Richard JC, Jaber S, Lemaire F, Brochard L. Alveolar derecruitment at decremental positive end-expiratory pressure levels in acute lung injury: comparison with the lower inflection point, oxygenation, and compliance. Am J Respir Crit Care Med. 2001. 164:795–801.25. Ward NS, Lin DY, Nelson DL, Houtchens J, Schwartz WA, Klinger JR, Hill NS, Levy MM. Successful determination of lower inflection point and maximal compliance in a population of patients with acute respiratory distress syndrome. Crit Care Med. 2002. 30:963–968.
Article26. Mergoni M, Martelli A, Volpi A, Primavera S, Zuccoli P, Rossi A. Impact of positive end-expiratory pressure on chest wall and lung pressure-volume curve in acute respiratory failure. Am J Respir Crit Care Med. 1997. 156:846–854.
Article27. Ranieri VM, Brienza N, Santostasi S, Puntillo F, Mascia L, Vitale N, Giuliani R, Memeo V, Bruno F, Fiore T, Brienza A, Slutsky AS. Impairment of lung and chest wall mechanics in patients with acute respiratory distress syndrome: role of abdominal distension. Am J Respir Crit Care Med. 1997. 156:1082–1091.28. Harris RS, Hess DR, Venegas JG. An objective analysis of the pressure-volume curve in the acute respiratory distress syndrome. Am J Respir Crit Care Med. 2000. 161:432–439.
Article29. Rimensberger PC, Cox PN, Frndova H, Bryan AC. The open lung during small tidal volume ventilation: concepts of recruitment and "optimal" positive end-expiratory pressure. Crit Care Med. 1999. 27:1946–1952.
Article30. Rimensberger PC, Pristine G, Mullen BM, Cox PN, Slutsky AS. Lung recruitment during small tidal volume ventilation allows minimal positive end-expiratory pressure without augmenting lung injury. Crit Care Med. 1999. 27:1940–1945.
Article31. Albaiceta GM, Luyando LH, Parra D, Menendez R, Calvo J, Pedreira PR, Taboada F. Inspiratory vs. expiratory pressure-volume curves to set end-expiratory pressure in acute lung injury. Intensive Care Med. 2005. 31:1370–1378.
Article32. Lu Q, Malbouisson LM, Mourgeon E, Goldstein I, Coriat P, Rouby JJ. Assessment of PEEP-induced reopening of collapsed lung regions in acute lung injury: are one or three CT sections representative of the entire lung? Intensive Care Med. 2001. 27:1504–1510.
Article33. Hickling KG. Best compliance during a decremental, but not incremental, positive end-expiratory pressure trial is related to open-lung positive end-expiratory pressure: a mathematical model of acute respiratory distress syndrome lungs. Am J Respir Crit Care Med. 2001. 163:69–78.34. Lim CM, Soon Lee S, Seoung Lee J, Koh Y, Sun Shim T, Do Lee S, Sung Kim W, Kim DS, Dong Kim W. Morphometric effects of the recruitment maneuver on saline-lavaged canine lungs. A computed tomographic analysis. Anesthesiology. 2003. 99:71–80.35. Romand JA, Shi W, Pinsky MR. Cardiopulmonary effects of positive pressure ventilation during acute lung injury. Chest. 1995. 108:1041–1048.
Article36. Pinsky MR. Cardiovascular issues in respiratory care. Chest. 2005. 128:592S–597S.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Positive end Expiratory pressure on the Pulmonary Capillary Pressure in Acute Lung Injury Patients
- Effect of Recruiting Maneuvers in a Patient with Acute Lung Injury after Femoral Nailing: A case report
- Intraocular Pressure during Mechanical Ventilation with Positive End-Expiratory Pressure under General Anesthesia
- Effects of Differential Lung Ventilation with Positive End-Expiratory Pressure on Ischemia-Reperfusion Lung Injury in Dogs
- The effect of positive-end expiratory pressure on oxygenation during high frequency jet ventilation and conventional mechanical ventilation in the rabbit model of acute lung injury